Diabetic ketoacidosis (DKA) is a relatively common complication of diabetes mellitus in dogs and cats. In the face of insulin deficiency or resistance, the liver produces ketones to provide an alternative energy source from glucose. However, excessive ketone production can lead to high anion gap metabolic acidosis and other negative effects. Besides restoration of intravascular and interstitial fluid deficits as well as electrolyte derangements such as hypokalemia, insulin administration is necessary to stop production of ketones, reduce lipolysis and enhance cellular uptake of glucose.
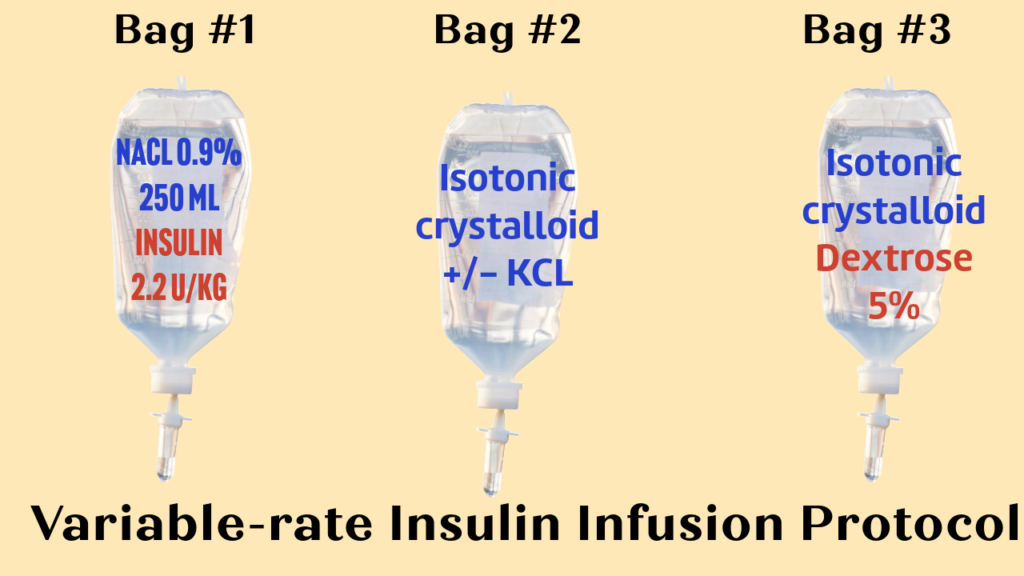
Several insulin protocols have been described in veterinary medicine to treat DKA patients during the first 24-72 hours of hospitalization until the patient becomes stable and regains appetite. One of the most commonly utilized protocols in clinical practice is an intravenous variable-rate insulin infusion protocol when a short-acting insulin is infused IV and the rate is altered based on blood glucose concentration (Figure 1).
| BG (mg/dL or mmol/L) | Intravenous fluid composition | Administration rate, ml/hr |
| >250 or >13.9 | 0.9% NaCl | 10 |
| 200-250 or 11.1-13.9 | 0.9% NaCl +2.5% Dextrose | 7 |
| 150-199 or 8.3-11.1 | 0.9% NaCl +2.5% Dextrose | 5 |
| 100-149 or 5.6-8.3 | 0.9% NaCl +5% Dextrose | 5 |
| <100 or <5.6 | 0.9% NaCl +5% Dextrose | Stop insulin |
Simultaneous administration of dextrose with insulin infusion enables veterinarians to administer higher insulin doses than those without dextrose supplementation. Insulin plays a crucial role in DKA therapy, ensuring the reduction of ketogenesis. When using the variable-rate insulin infusion protocol, it is recommended to include either 2.2 units per kg for dogs or 1.1 units per kg for cats of regular insulin into the 250 ml bag of normal saline which translates to ~0.045-0.09 U/kg/hr of insulin supplementation if the fluid is run at the rate of 10 ml/hr. A lower dosage of insulin for cats (1.1 U/kg/day [0.045 U/kg/hr] vs. 2.2 U/kg/day [0.09 U/kg/hr]) is occasionally recommended because of a suspected higher risk for neurologic adverse effects from rapid correction of hyperglycemia in this species, however the evidence-based research proving this hypothesis is lacking. A 2010 study (Clauss et al., JVECC) reported treating cats with a canine insulin dosage of 2.2 U/kg/day. No increased frequency of adverse neurological or biochemical events was observed when employing a sliding scale to restrict the amount of insulin administered to the cats. Therefore, in theory, higher canine doses of intravenous insulin could be considered for cats.
The variable-rate insulin infusion protocol can be challenging to implement due to the need for frequent adjustments in both insulin and dextrose rates based on blood glucose levels. As a result, the use of the protocol may increase the risk of human errors. In addition, it is not uncommon when DKA patients don’t receive the full daily dose of insulin due to relatively low blood glucose levels despite dextrose supplementation. These disruptions in the administration of insulin may impede the resolution of ketonemia and acidemia. In the previously mentioned feline study (Clauss et al., JVECC 2010), the use of a sliding scale for determination of infusion rates significantly reduced the amount of insulin cats received in this setting. They found that only 24%–35% of the daily prescribed insulin dose was actually administered.
Since the variable-rate infusion protocol is not perfect, are there any alternatives?
Despite the lack of randomized controlled trials in human patients, there has been a consensus shift towards managing DKA using a fixed-rate intravenous insulin infusion (FRI). This involves the continuous administration of insulin at a fixed rate, with the option to separately add dextrose infusion to regulate blood glucose concentration within a specific range.
In the most recent prospective randomized study performed by Gant et al. (JVECC 2024), the authors compared an FRI protocol to a variable-rate (VRI) protocol in dogs and cats. They recruited both dogs and cats presenting to a university teaching hospital or a private referral practice and were diagnosed with DKA based on the following criteria:
- Venous blood pH <7.3
- BG > 11 mmol/l (>198 mg/dl)
- Ketonemia >3 mmol/L (β-hydroxybutyrate)
Patients were assigned to receive either fixed-rate or variable-rate insulin infusion protocol by randomization.
For the fixed-rate insulin infusion protocol, 3 bags were pre-made:
Bag #1: Contained 50 units of regular insulin added to a 500 ml bag of NaCl 0.9%, resulting in a concentration of 0.1 U of insulin per ml of solution.
Bag #2: An isotonic crystalloid solution, was used to correct dehydration and provide maintenance rates.
Bag #3: A 500 ml isotonic crystalloid solution, had 50 ml of dextrose 50% added to create a final 5% dextrose solution. If needed, the dextrose concentration could be increased to 10% to prevent hypoglycemia. In this case, an infusion via a central line was recommended. Potassium chloride could be added to either or both bags #2 and #3 as needed to correct hypokalemia.

According to the fixed-rate insulin protocol, the suggested rates for insulin, dextrose, and fluid were as follows:
- BG >15 mmol/L (>270 mg/dL): The patient received insulin from bag #1 at a rate of 1 ml/kg/hr, equivalent to 0.1 U/kg/hr of insulin supplementation, along with fluid from bag #2 to correct dehydration and provide maintenance as needed.
- BG = 7-15 mmol/L (126-270 mg/dL): The patient received insulin from bag #1 at a rate of 1 ml/kg/hr (=0.1 U/kg/hr) in addition to the fluid from bag #3, containing 5% dextrose. The fluid rate of dextrose-containing solution could be as low as 2 ml/kg/hr or higher to correct dehydration and any ongoing losses as well as maintain BG within the 7-15 mmol/L range.
- BG <7 mmol/L (<126 mg/dL): Insulin administration was halted, and only the fluid from bag #3 (dextrose 5%) was continued at an appropriate rate determined by an attending clinician.
For the variable-rate infusion, 3 bags were premade as well:
Bag #1: The insulin bag – contained 2.2 U/kg of insulin added to a 250 ml bag of NaCl 0.9% for both dogs and cats.
Bag #2: An isotonic crystalloid solution used to correct dehydration and provide maintenance rates.
Bag #3: A 500 ml isotonic crystalloid solution that had 50 ml of dextrose 50% added to create a final 5% dextrose solution. Potassium chloride could be added to either or both bags #2 and #3 as needed to correct hypokalemia.
The following modified sliding scale was then used to adjust the insulin infusion based on BG concentration as depicted in the table below (Figure 4):
| Blood Glucose:(mmol/L) [mg/dL] | Bag#1: Insulin Bag (ml/h) | Bag #2: Isotonic fluids +/- KCl(ml/kg/h) | Bag #3: 5% Dextrose +/- KCl(ml/kg/h) |
|---|---|---|---|
| >15 [270] | 10 | 2+ | Stop |
| 12-14.9 [216 – 269] | 7 | 2+ | 2 |
| 8-11.9 [144 – 215] | 5 | 2+ | 2 |
| 5-7.9 [90-214] | 5 | 2+ | 4 |
| <5 [90] | 0 | 2+ | 4 |
In both protocols, insulin infusion bags and lines were changed every 24 hours and lines were primed with 50 mL of insulin solution to allow for insulin adsorption to plastic. The duty clinician could increase the insulin infusion rate in the presence of persistent hyperglycemia or ketonemia; however, this was not protocolized.
The resolution of ketosis was defined as the decrease in β-hydroxybutyrate [BHB] concentration below 0.6 mmol/L as determined by the point-of-care ketone analyzer – FreeStyle Optium Neo H-ketone meter manufactured by Abbott Laboratories in the UK (Figure 5).

So, what were the results of this study?
First, we are going to focus on the feline arm of this study.
A total of 16 cats underwent the final statistical analysis (8 cats in the fixed rate infusion protocol and 8 cats in the variable rate protocol). The baseline characteristics such as age, sex, weight, breeds, probability of mortality based on the APPLE score, baseline BHB concentration, baseline blood pH, time to initiation of insulin therapy in both groups were relatively similar with no significant differences. In both groups, urinary system disorders and pancreatitis were the most common comorbidities.
The baseline mortality probability based on the APPLE score in the variable-rate infusion group was 73% vs. 40% in the fixed-rate infusion group meaning that cats in the VRI group were overall sicker, however this difference didn’t reach statistical significance with P=0.11. One should remember that when the sample size is very low, such as in this study with only 8 cats included in each group, the risk of the type 2 error – in other words false negative results of the statistical test – is relatively high. When comparing effects of an intervention (the insulin infusion protocol in this case), it is important to ensure that both study groups were relatively equal at baseline in terms of the severity of their disease (i.e. you want to compare ‘apples to apples’ as opposed to ‘apples to oranges’). Otherwise, you won’t be able to tease out the effect of the specific intervention versus the confounding effects of their underlying disease.
Now let’s directly compare the performance of both protocols in cats:
- 5 of 8 cats in the FRI group vs. 4 of 8 cats in the VRI group achieved the resolution of ketonemia, which was not statistically significant.
- There was no statistical difference in terms of the time of resolution of ketonemia in both groups: 48 hours in the FRI group vs. 37 hours in the VRI group. Note: the study was powered to detect the time difference of greater than 14 hours only. Therefore, the lack of statistical significance could have been a false negative result.
- None of the cats in both groups developed hypoglycemia with BG less than 4.5 mmol/L or 81 mg/dl.
- 4 cats on FRI and 2 cats on VRI protocols had BG concentration measured below 7 mmol/L (126 mg/dL), necessitating temporary cessation of insulin administration.
- Overall insulin rate until resolution of ketonemia was similar in both groups: with mean values of 0.1 unit/kg/hr in the FRI group and 0.09 u/kg/hr in the VRI group.
- Cats in the FRI group spent on average 6.9 days in the hospital until they were discharged vs. 5 days in the VRI group. The authors were unable to determine the statistical difference between the groups due to the low number of cats that were discharged home.
- Overall, 6/8 of the cats in the FRI group, and 5/8 cats in the VRI groups were successfully discharged home.
Based on these results, the performance of both protocols in cats was relatively equal with the caveat that the sample size was quite low and the statistical difference could have been missed.
Now, we are going to switch gears and talk about the canine arm of the study.
A total of 20 dogs underwent the final statistical analysis (10 dogs in the fixed-rate infusion protocol and 10 dogs in the variable-rate protocol). Similar to cats, the baseline characteristics were relatively equal with no significant differences reported. In both canine groups, urinary system disorders such as kidney disease and/or UTI and pancreatitis were the most common comorbidities. The mortality probability based on the APPLE score in the VRI group was 42% vs. 13% in the FRI group with P=0.32.
Now, let’s directly compare the performance of the two study protocols in dogs:
- 9 of 10 dogs in the FRI group vs. 10 of 10 dogs in the VRI group achieved the resolution of ketonemia, which was not statistically significant.
- There was no statistical difference in terms of the time of resolution of ketonemia in both groups: 31.8 hours in the FRI group vs. 25.1 hours in the VRI group (P=0.89). Note: the study was powered to detect the time difference of greater than 14 hours only. Therefore, the lack of statistical significance could have been a false negative result.
- None of the dogs in both groups developed hypoglycemia with BG less than 4.5 mmol/L or 81 mg/dl.
- 3 dogs on FRI and 2 dogs on VRI protocols had BG concentration measured below 7 mmol/L (126 mg/dL), necessitating temporary cessation of insulin administration.
- Overall insulin rate until resolution of ketonemia was higher in the FRI group compared with the VRI group with the mean values of 0.1 unit/kg/hr vs. 0.08 u/kg/hr, respectively. This was statistically different with the P value of 0.04.
- Dogs in the FRI group spent significantly less time in the hospital and were discharged on average after 5.4 days of hospitalization vs. 8.3 days in the VRI group. The P value for this difference was 0.005.
- 8 of the 10 dogs in the FRI group, and 6 of 10 dogs in the VRI group were successfully discharged home, however this was not statistically different (P=0.63).
Based on these results, the overall performance of both protocols was relatively similar, however the dogs receiving fixed-rate insulin infusion went home 3 days earlier, which is both clinically and statistically significant.
TAKEAWAYS
- It was a well-conducted randomized clinical trial that directly compared the fixed-rate insulin infusion protocol with the variable-rate insulin infusion protocol in both dogs and cats. Although the authors did a great job to ensure that the study groups were relatively equal at the baseline, the study population was still small and therefore prone to heterogeneity that could have confounded the final results. In addition, the sample size calculation was performed only to detect the difference in time of resolution of ketonemia of greater than 14 hours, and none of the other variables were taken into account to calculate the sample size. Therefore, the final results of this study should be interpreted cautiously and further research is required to make more definitive conclusions.
- In this study, ketosis resolved in 19 of 20 (or 95%) dogs with an overall mean time to resolution of 27.8 hours. On the other hand, ketosis resolved only in 9 of 16 cats (56.3%) with an overall median time to resolution of 72 hours. All cats that died (5/16 or 31.3%) failed to achieve resolution of ketosis. It is important to note that in this study, resolution of ketosis was defined as blood BHB concentration <0.6 mmol/L. In other studies, resolution criteria have included undetectable urine or serum acetoacetate or serum BHB concentration <1-2.55. Semi-quantitative urine test strips only measure acetoacetate, however their serum concentrations are relatively lower than BHB in DKA, therefore they are no longer considered appropriate for determining resolution of ketosis.
- In this patient population, there was not a clinically significant difference in time to resolution of ketosis in cats and dogs with DKA receiving insulin by an FRI or a VRI. However, dogs, randomized to an FRI protocol had a shorter length of hospitalization, but the fact that resolution of ketosis was not significantly faster compared to the VRI group suggests other factors may be more important for the length of hospitalization (for example, the presence of comorbidities such as aspiration pneumonia and pancreatitis).
The Bottom Line
In my view, both fixed-rate and variable-rate insulin infusion protocols are viable for treating dogs and cats with DKA. However, based on current evidence, neither protocol demonstrates superiority in clinically relevant outcomes. While there’s a potential indication that the fixed-rate insulin protocol could lead to shorter hospitalization in dogs, further research is needed to validate these findings. Personally, I find the fixed-rate insulin protocol to be somewhat more straightforward in implementation, requiring fewer adjustments in insulin infusion rates compared to the variable-rate infusion protocol. Nevertheless, it may necessitate increased dextrose supplementation. The 3-bag technique described in the Gant et al. study is highly intuitive and is worth consideration when prescribing insulin infusion for DKA patients.
References
Claus, M. A., Silverstein, D. C., Shofer, F. S., & Mellema, M. S. (2010). Comparison of regular insulin infusion doses in critically ill diabetic cats: 29 cases (1999-2007). Journal of veterinary emergency and critical care (San Antonio, Tex. : 2001), 20(5), 509–517. https://doi.org/10.1111/j.1476-4431.2010.00567.x
Gant, P., Barfield, D., & Florey, J. (2024). Comparison of insulin infusion protocols for management of canine and feline diabetic ketoacidosis. Journal of veterinary emergency and critical care (San Antonio, Tex. : 2001), 34(1), 23–30. https://doi.org/10.1111/vec.13354

Hi i think that i saw you visited my web site thus i came to Return the favore I am attempting to find things to improve my web siteI suppose its ok to use some of your ideas
you are in reality a good webmaster The website loading velocity is amazing It sort of feels that youre doing any distinctive trick Also The contents are masterwork you have done a fantastic job in this topic.
먹튀검증 커뮤니티 먹튀감별사
온라인 카지노 | 토토 사이트 먹튀 방지
[토토사이트 추천] 함께 나누는 온라인 안전 놀이터 정보!
Totally agree with this! The article is on point.
Magnificent beat I would like to apprentice while you amend your site how can i subscribe for a blog web site The account helped me a acceptable deal I had been a little bit acquainted of this your broadcast offered bright clear idea
I was suggested this web site by my cousin. I’m not sure whether this post is written by him as no one else know such detailed about my trouble. You are incredible! Thanks!
of course like your website but you have to check the spelling on several of your posts A number of them are rife with spelling issues and I in finding it very troublesome to inform the reality on the other hand I will certainly come back again
What a remarkable article! The way you’ve tackled the topic with such precision and depth is commendable. Readers are sure to gain a great deal from the wealth of knowledge and practical insights you’ve shared. Your profound understanding of the subject shines through every part of the piece. I’m eager to see more of your exceptional work. Thank you for offering your expertise and providing us with such enlightening and comprehensive content.
빠르고 안전한 먹튀검증 전문 커뮤니티 먹튀감정사를 이용하세요.
The degree of my admiration for your work is just as great as your personal opinion. Your visual presentation is elegant, and the authored content is both fashionable and interesting. However, it appears that you are apprehensive of delivering something that may be seen as dubious. I believe that we will be able to resolve this issue quickly and effectively.
”
토토검증 사이트는 토토샵
먹튀검증 사이트는 토토샵
https://toto-shop.net
“
Ny weekly I just like the helpful information you provide in your articles
Your perspective adds a lot to the discussion—well done!
Hi, I’m Jack. Your blog is a treasure trove of valuable insights, and I’ve made it a point to visit daily. Kudos on creating such an amazing resource!
Hey, Jack here. I’m hooked on your website’s content – it’s informative, engaging, and always up-to-date. Thanks for setting the bar high!
Tech to Force I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
Your blog is a true hidden gem on the internet. Your thoughtful analysis and in-depth commentary set you apart from the crowd. Keep up the excellent work!
Aroma Sensei I just like the helpful information you provide in your articles
I do trust all the ideas you’ve presented in your post. They are really convincing and will definitely work. Nonetheless, the posts are too short for newbies. May just you please lengthen them a bit from next time? Thank you for the post.