Hyperkalemia has been reported as a complication of general anesthesia in systemically healthy animals with normal renal function. Several case reports and case series are summarized in Table 1. Upon reviewing the literature, several distinct patterns and interesting observations are worth discussing. Some of these observations may be relevant to veterinary practitioners and technicians dealing with anesthetized animals or managing their post-anesthetic recovery.
Species and Breeds
Anesthesia-associated hyperkalemia was originally reported in large non-domesticated cats; however, recently, several case reports documented this phenomenon in dogs as well. Only one case report described a domestic short-haired cat who developed acute severe hyperkalemia under general anesthesia. Among dogs, Greyhounds are overrepresented; however, other breeds (e.g., Siberian Husky, German Shepherd Dog, Dogue de Bordeaux, Rottweiler, Whippet, and Labrador) have also been reported. Based on this breed distribution, we may hypothesize that medium to large breed dogs may have an increased risk of anesthesia-induced hyperkalemia.
In an unpublished study (presented as an abstract only), authors described a cohort of healthy Greyhounds that had a high prevalence of hyperkalemia during general anesthesia: 36 out of 95 (38%) dogs had serum potassium >5.6 mmol/L and normal baseline serum potassium prior to general anesthesia.
Etiology of Hyperkalemia Associated with General Anesthesia
That’s where things get interesting. The short answer is that nobody knows exactly why different species of animals develop very acute severe hyperkalemia (K+=8-9 mmol/L) under general anesthesia. It is likely multifactorial, and several theories have been discussed in the literature. Before we discuss possible causes of this phenomenon, let’s quickly recap the most common groups of causes of hyperkalemia development in animals and people.
Hyperkalemia can be caused by three different mechanisms:
1. Increased potassium load
2. Decreased renal potassium excretion
3. Transcellular shift
Hyperkalemia diagnosed in all published reports was most likely caused by either transcellular potassium shift or, less likely, decreased renal potassium excretion. Almost all described animals had normal renal values, and many of them had normal ACTH stimulation test results or baseline cortisol, ruling out Addison’s disease. An increased potassium load can be effectively ruled out because none of these cases were receiving a considerable amount of potassium-containing solutions.
The transcellular potassium shifting (from intracellular space to the extracellular space) makes perfect sense because severe hyperkalemia developed and resolved very quickly in the majority of described animals.
Several factors can lead to a shift of potassium from the intracellular space to the extracellular space (see Figure 1):
- Cell Lysis or cellular injury/damage: Destruction of cells, such as in hemolysis, tumor lysis syndrome, or rhabdomyolysis, or cellular damage secondary to trauma and burns can release intracellular potassium into the bloodstream.
- Increased metabolic rate secondary to hyperthermia and exercise can cause depletion of ATP molecules and a temporary shift of potassium from cells to the extracellular space.
- Hyperosmolarity of the extracellular space may lead to a drag of water and potassium from the intracellular space.
- Insulin deficiency may lead to reduced activity of Na/K ATPase pumps, leading to the lack of potassium uptake into the cells.
- Acidosis: An increase in hydrogen ions (decrease in pH) can lead to the movement of potassium out of cells.
- Medications: Medetomidine primarily acts on alpha-2 adrenergic receptors; alpha-2 adrenergic receptor activation can inhibit insulin release from the pancreas. Insulin facilitates the movement of potassium into cells, and reduced insulin levels can contribute to an elevation of extracellular potassium. The inhibition of insulin release and the reduction in sympathetic nervous system activity can lead to decreased cellular uptake of potassium by various tissues, including muscle cells.

As evident from Table 1, the majority of non-Greyhound dogs and non-domesticated cats received medetomidine. Medetomidine, an alpha-2-agonist, reduces aldosterone secretion by decreasing circulating catecholamine levels, achieved through a decrease in sympathetic tone and a direct impact on the RAAS system. Demonstrated to cause a dose-dependent, centrally mediated decrease in sympathetic outflow by inhibiting the release of catecholamines, this effect persists up to 3 hours after a single dose. Consequently, with reduced circulating catecholamine levels, there may be an imbalance in the activation of adrenergic receptors, favoring the stimulation of α-adrenoceptors. This imbalance promotes a greater efflux of potassium from the cell. Furthermore, alpha-2 adrenergic receptor activation can inhibit insulin release from the pancreas, and reduced insulin levels can contribute to an elevation of extracellular potassium. After the administration of medetomidine, plasma insulin levels can be significantly decreased for up to 120 minutes post-injection due to direct action on α-2 adrenoceptors on pancreatic islet β cells.
In the study by Louro et al., they described six dogs that were not Greyhounds and developed severe hyperkalemia during general anesthesia. All of them received medetomidine, and hyperglycemia occurred in five dogs, supporting the hypothesis that insulin release suppression played a role in the development of hyperkalemia.
In contrast, in most papers describing Greyhounds with hyperkalemia under general anesthesia, the majority of these dogs remained euglycemic throughout anesthesia. Neither dog received an α2-adrenergic receptor agonist, except for the two case reports (Pye et al. and McFadzean et al.) where two dogs received dexmedetomidine. Based on this information, we may conclude that the use of α2-adrenergic receptor agonists doesn’t play a significant role in the development of hyperkalemia in Greyhounds compared to other breeds.
Another potential cause of the transcellular shift of potassium under general anesthesia may include hyperthermia and acidosis; however, they were not present in all reported dogs. Hyperthermia (>40°C) was identified in three of the six dogs described by Louro et al. Severe hyperthermia (>41.6°C) can result in cellular structural damage and enzymatic impairment, leading to cell death and consequent release of intracellular potassium.
Acidemia causes efflux of potassium from cells by diminishing sodium–potassium–ATPase activity, binding of protons to negatively charged cellular proteins, and pH-sensitive potassium channels. Mineral metabolic acidosis (e.g., NH4Cl) causes the greatest efflux of potassium from cells. Organic acidosis (e.g., secondary to hyperlactatemia) may be accompanied by hyperkalemia, but the pathophysiology may not directly involve acidemia. In anesthetized dogs, changes in PaCO2 caused small increases in plasma potassium levels (0.39 mmol/L for every 7.5-mmHg increase in PaCO2), although this was not clinically relevant, and no ECG abnormalities were detected (Hassan et al, 1979).
Another condition that have been reported in children and adults is anesthesia-induced rhabdomyolysis or AIR (Gray, Pediatric anesthesia 2017). It is believed to be an idiosyncratic reaction that may be induced by exposure to halogenated agents (including isoflurane and sevoflurane). AIR may share some features with malignant hyperthermia, however the body temperature may be normal. Patients with AIR may develop sudden ECG changes during general anesthesia, and their bloodwork shows severe hyperkalemia similar to veterinary reports. Unfortunately, none of the canine or feline cases described in aforementioned reports, had creatine kinase (CK) levels measured that could have helped to rule in or out this differential diagnosis.
Based on the published literature, the exact cause of hyperkalemia associated with general anesthesia remains unclear. It is likely multifactorial and may include the use of certain drugs (e.g., alpha-2-agonists or inhalant anesthesia), acidemia, hyperthermia, genetic predisposition (e.g., Greyhounds), anesthesia-induced rhabdomyolysis and other causes that are not identified yet.
How can you recognize the acute development of hyperkalemia in an anesthetized patient?
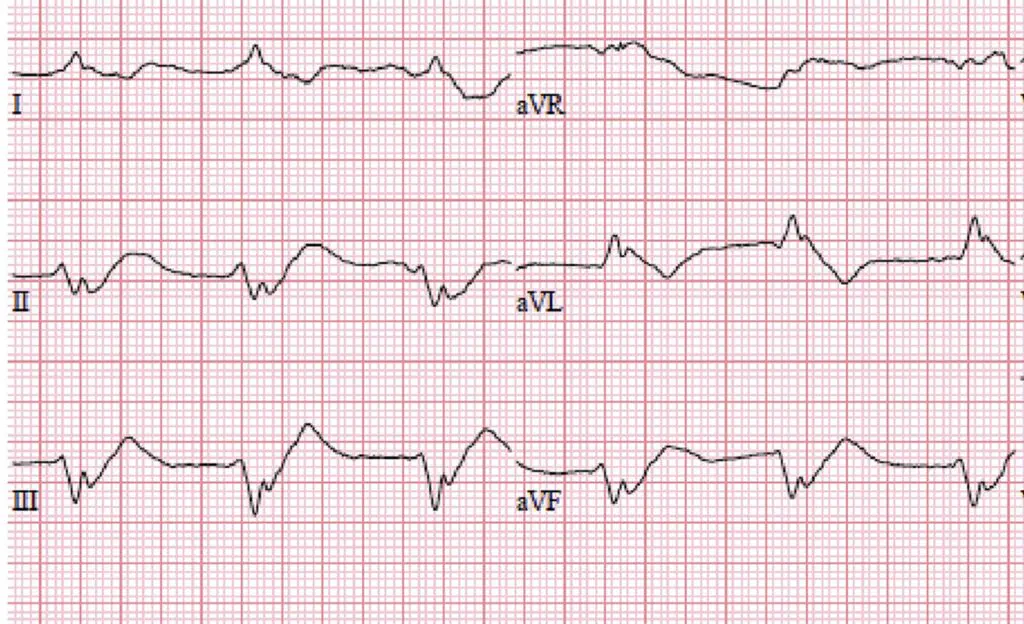
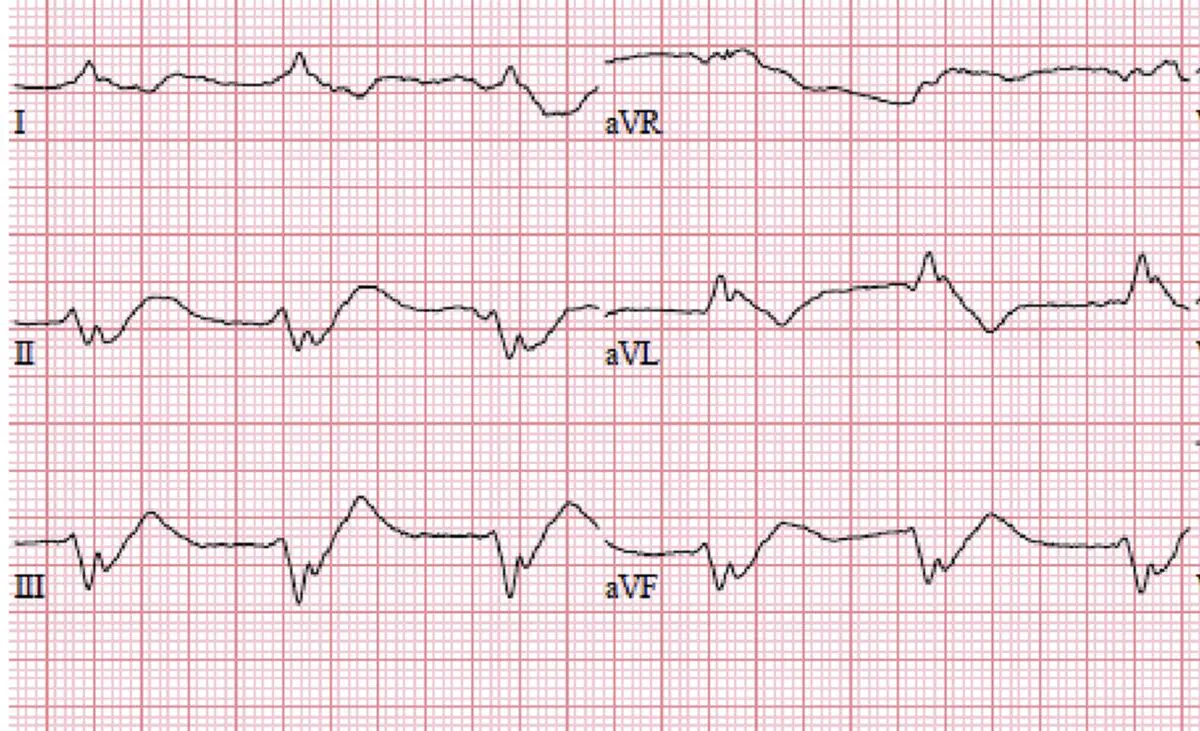
The most common scenario described in the aforementioned papers was that an anesthetized patient experienced an acute reduction in heart rate (e.g., from 120 to 40-50 bpm) and developed ECG changes characteristic of severe hyperkalemia (sinoventricular rhythm, atrial standstill, tall T waves). These changes were accompanied by decreased blood pressure and abnormal perfusion parameters. The onset of these changes varied, but the most common timing was 125 minutes (ranging from 70 to 170 minutes) from premedication and 74 minutes (ranging from 45 to 125 minutes) post-induction. Once these changes were detected, a clinician would perform a venous blood gas analysis that showed severe hyperkalemia (range, 6-9 mmol/L).
How were these cases managed?
The management of these cases varied from paper to paper. Dogs that received alpha-2-agonists were commonly reversed with atipamezole. Some of these dogs received a 10-20 ml/kg fluid bolus due to arterial hypotension, and calcium gluconate was administered to address their ECG changes. In cases where the dog was doing poorly from a cardiovascular standpoint, general anesthesia was discontinued. Dogs that were hypoventilating (i.e., had hypercapnia) were started on mechanical ventilation to control their CO2 levels. Hyperkalemia was treated with the administration of dextrose, insulin, and B2-agonists in some cases. Some of these animals received atropine or glycopyrrolate, but they did not show improvement in bradycardia. Anticholinergics may be ineffective in treating severe bradycardia induced by hyperkalemia because high potassium reduces myocardial excitability, suppresses sinoatrial node activity, and impairs conduction at the atrioventricular node. This reduces the response to anticholinergic drug administration. Based on this, we may conclude that when an animal presents with atropine-resistant bradycardia, hyperkalemia should be considered (Louro et al. 2020).
The Bottom Line
- Acute severe hyperkalemia may develop in dogs and cats under general anesthesia, even if these patients had normal baseline potassium levels and were systemically healthy.
- Sudden bradycardia with associated ECG changes (sinoventricular rhythm, atrial standstill, tall T waves) is a common finding in reported cases.
- Medetomidine and other alpha-2 agonists appear to be a common factor in all non-Greyhound cases reported. There are several mechanisms in which medetomidine may play a role in the development of hyperkalemia during general anesthesia.
- Other factors, such as a combination of certain drugs, acidemia, anesthesia-induced rhabdomyolysis and hyperthermia, may also play a role.
- Other cases of hyperkalemia during general anesthesia have been reported in patients who did not receive medetomidine (the majority of them were Greyhounds).
- Since many of these animals developed hyperkalemia 1-2 hours after induction, conserving anesthesia time as much as possible and considering staging or splitting procedures into smaller anesthetic events on different days may be beneficial.
- Consistent monitoring of ECG, blood pressure, capnography, SpO2, and temperature is vital to detect the onset of hyperkalemia.
References
Louro, L.F., Raszplewicz, J. and Alderson, B. (2020), Hyperkalaemia during general anaesthesia: six cases. Vet Rec Case Rep, 8: e001075. https://doi.org/10.1136/vetreccr-2020-001075
Jones SJ, Mama KR, Brock NK, Couto CG. Hyperkalemia during general anesthesia in two Greyhounds. J Am Vet Med Assoc. 2019 Jun 1;254(11):1329-1334. doi: 10.2460/javma.254.11.1329. PMID: 31067178.
Boustead, K.J. and Zeiler, G. (2019), Life-threatening hyperkalaemia in a five-year-old rottweiler undergoing bilateral elbow arthroscopy. Vet Rec Case Rep, 7: e000893. https://doi.org/10.1136/vetreccr-2019-000893
Pye E, Ward R. Hyperkalaemia in a greyhound under general anaesthesia. Vet Rec Case Rep. 2023; 11:e585. https://doi.org/10.1002/vrc2.585
Felisberto, R., Auckburally, A. and Flaherty, D. (2020), Life-threatening hyperkalaemia during general anaesthesia in a domestic short-haired cat. Vet Rec Case Rep, 8: e001243. https://doi.org/10.1136/vetreccr-2020-001243
Reilly S, Seddighi MR, Steeil JC, Sura P, Whittemore JC, Gompf RE, Elliott SB, Ramsay EC. Selected clinical, biochemical, and electrolyte alterations in anesthetized captive tigers (Panthera tigris) and lions (Panthera leo). J Zoo Wildl Med. 2014 Jun;45(2):328-34. doi: 10.1638/2013-0202R.1. PMID: 25000694.
Hassan H, Gjessing J, Tomlin PJ. Hypercapnia and hyperkalaemia. Anaesthesia. 1979 Oct;34(9):897-9. doi: 10.1111/j.1365-2044.1979.tb08543.x. PMID: 161143.

Fantastic read! I was especially impressed by the depth provided on the topic, offering a perspective I hadn’t considered. Your insight adds significant value to the conversation. For future articles, it would be fascinating to explore more to dive deeper into this subject. Could you also clarify more about the topic? It caught my interest, and I’d love to understand more about it. Keep up the excellent work!
먹튀검증 커뮤니티 먹튀검증소 바로가기 : eatandrun.net
พิ่ม Impression (การมองเห็น) จาก User มากขึ้น บางคนอาจคิดว่าแค่มีโปรโฟล์ มีเพจใน Facebook แล้วลูกค้าจะเข้ามาสนใจสินค้าเองก็มีโอกาสเป็นไปได้อยู่บ้าง ปั้มไลค์เฟสแต่คงจะดีกว่าหากคุณมีใช้บริการ ปั้มไลค์เฟส นอกจากจะช่วย ปั้มไลค์ ให้คุณมียอดไลค์ล้นหลามแล้ว ยังเพิ่มการมองเห็นทำให้ลูกค้าเกิดความสนใจเข้ามาซื้อสินค้ามากกว่าเดิม ทำให้มี Reliable (มีความน่าเชื่อถือ) ในการนำเสนอสินค้า หากคุณเพิ่งมีหน้าร้านออนไลน์อย่าง
Magnificent beat I would like to apprentice while you amend your site how can i subscribe for a blog web site The account helped me a acceptable deal I had been a little bit acquainted of this your broadcast offered bright clear idea
I just wanted to drop by and say how much I appreciate your blog. Your writing style is both engaging and informative, making it a pleasure to read. Looking forward to your future posts, especially on traffic increase!
My enthusiasm for your work has matched my own. Your visual presentation is polished, and the high-quality content you’re producing is admirable. However, you appear to be concerned about the possibility of delivering something that will cause anxiety. I’m aware that you’ll be able to address this issue quickly.
Your blog is a breath of fresh air in the crowded online space. I appreciate the unique perspective you bring to every topic you cover. Keep up the fantastic work!
of course like your website but you have to check the spelling on several of your posts A number of them are rife with spelling issues and I in finding it very troublesome to inform the reality on the other hand I will certainly come back again
real estate agents near me
Sky Scarlet Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated