In the field of veterinary medicine, standard clotting tests like prothrombin time (PT) and partial thromboplastin time (PTT) have traditionally been used to diagnose hypocoagulability, or a decreased ability of the blood to clot. However, recent research has raised the question of whether both prolonged and shortened PT/PTT can actually be indicative of hypercoagulability, a state where there is an increased tendency for blood clot formation.
Continue reading “Can both prolonged PT/PTT and shortened PT/PTT be indicative of a prothrombotic state?”Galleries
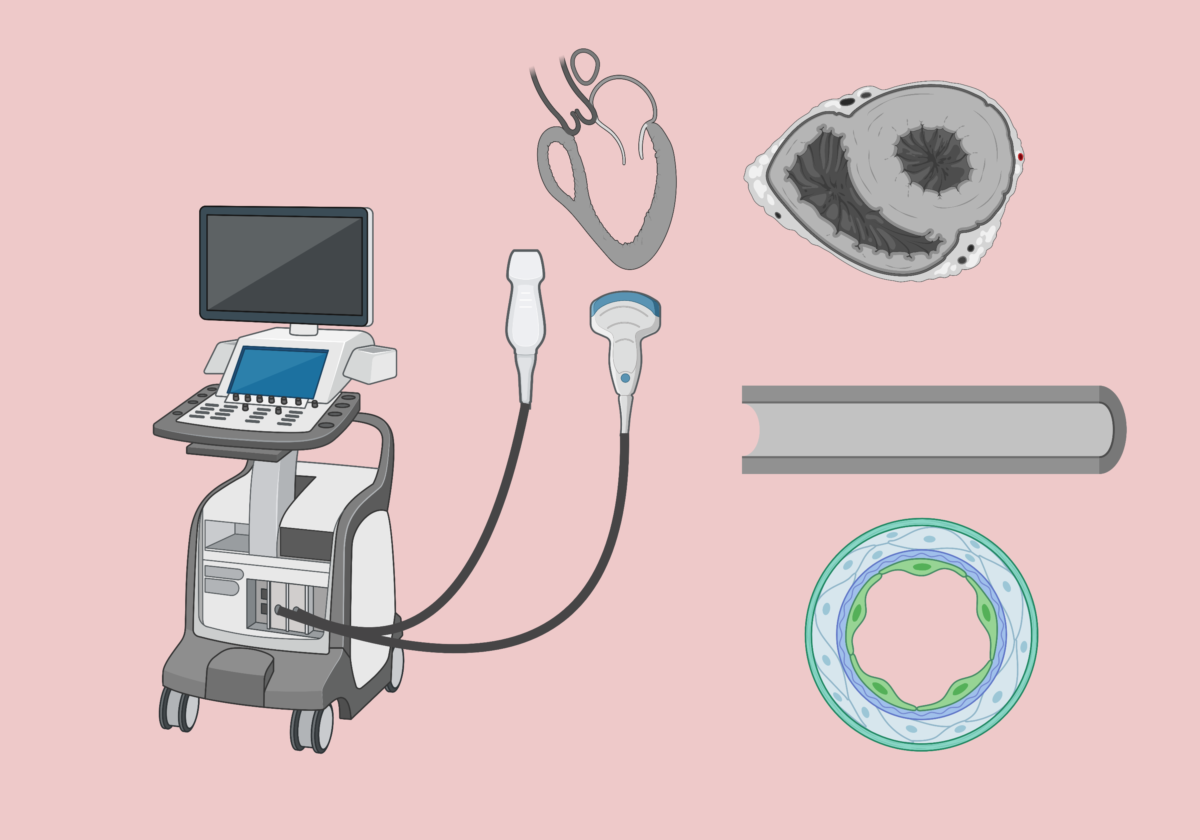
Assessment of the intravascular volume status with point-of-care ultrasound
Assessment of the intravascular volume status is a critical skill for emergency veterinarians. Point-of-care ultrasonography (POCUS) is emerging as a valuable, noninvasive, cage-side diagnostic tool for objective evaluation of physiologic and hemodynamic parameters related to volume status, fluid tolerance, and responsiveness. Rapid cage-side sonographic evaluation can obtain qualitative data on cardiac function even when performed by non-cardiologists. POCUS involves answering focused clinical questions using cage-side ultrasonography and increases the sensitivity of the conventional physical examination.
That said, POCUS findings should be interpreted in conjunction with other clinical parameters—such as conventional perfusion parameters (heart rate, mentation, body temperature, mucous membrane color, CRT, pulse quality), urine output, blood pressure, and body weight —and not viewed as an alternative to physical examination or standard imaging studies.
In this blog post, I will describe the most commonly used views to assess volume status in dogs and cats: focused sonographic assessment of the heart (cardiac POCUS) and caudal vena cava (CVC POCUS).
Continue reading “Assessment of the intravascular volume status with point-of-care ultrasound”Refeeding syndrome in dogs and cats
Refeeding syndrome refers to a potentially fatal constellation of metabolic derangements that occur upon refeeding a patient with an extended period of complete anorexia or severe malnutrition (Crook 2001; Kraft 2005). These metabolic derangements include severe hypophosphatemia, hypomagnesemia, hypokalemia, hyponatremia, hypocalcemia, hyperglycemia and vitamin deficiencies (Skipper 2012).
Continue reading “Refeeding syndrome in dogs and cats”High blood lactate in dogs and cats: good or bad???
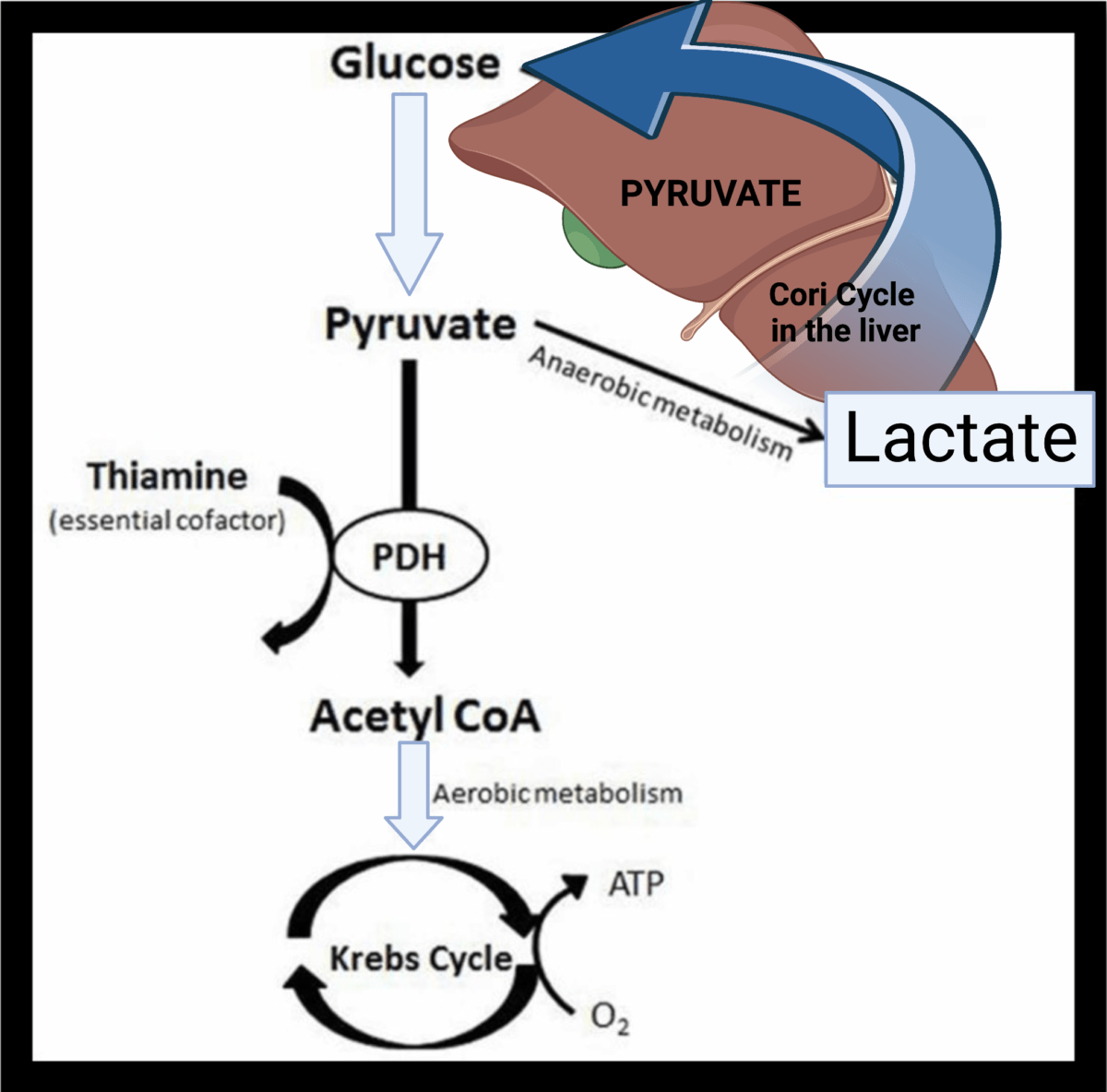
A lot of clinicians continue to believe that impaired tissue oxygenation is the main cause of increased blood lactate, and lactate itself results in metabolic acidosis. This biochemical understanding has persisted for long time, but there are some good reasons to challenge these traditional views on the ‘bad’ lactate.
After its production by anaerobic glycolysis lactate is re-used in the liver and the kidneys, and it may be converted back to glucose. The important point though is that lactate is also produced via aerobic glycolysis as a response to catecholamine release and stress. This may happen in septic patients, albuterol toxicity, trauma and other critical illnesses. In these clinical scenarios, the trigger for lactate production is adrenergic stimulation and not lack of oxygen.
If you want to learn more about lactate metabolism, watch this short video below:
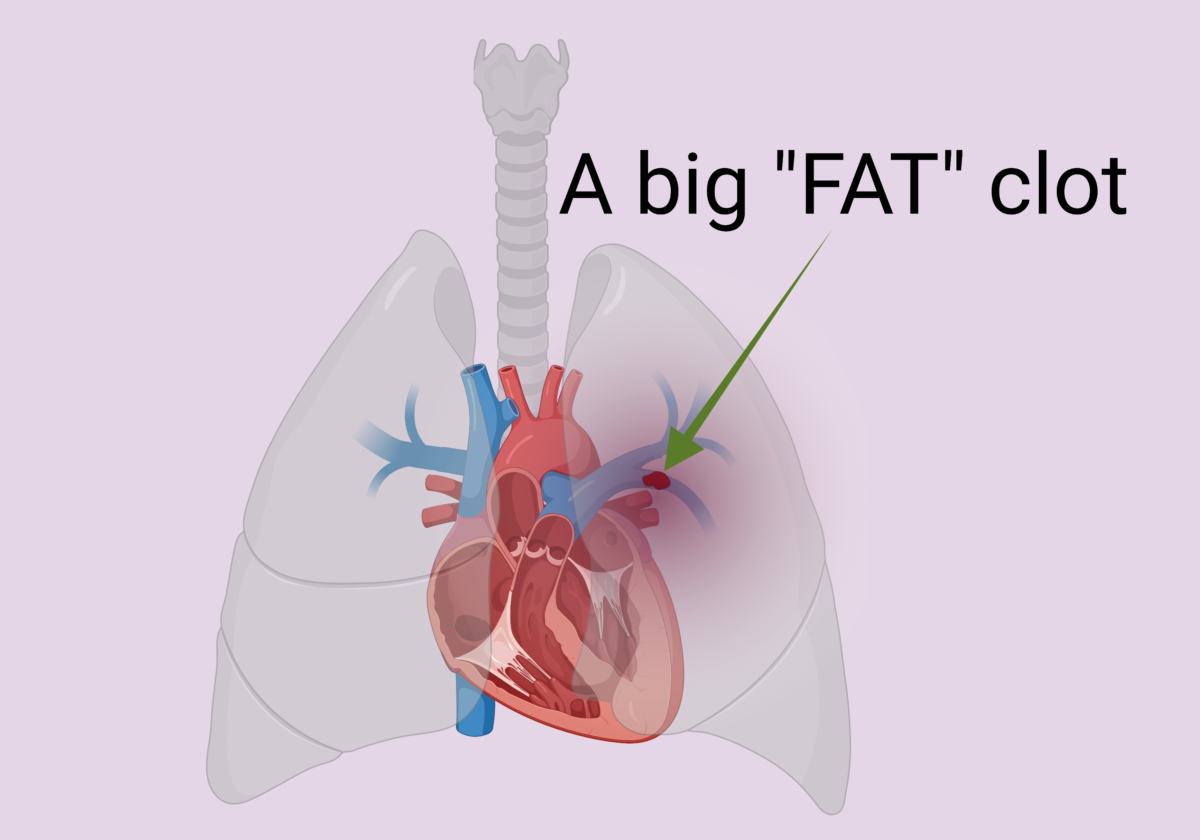
Pulmonary thromboembolism in dogs and cats: to lyse or not to lyse?
An 8-year-old neutered male dachshund was presented to the emergency department for evaluation of respiratory distress. The dog was previously diagnosed with a heartworm disease and was currently undergoing treatment with a “slow kill” method. Physical examination revealed tachycardia at 160/min, right-sided pulmonary crackles, and tachypnea with increased respiratory effort. The point-of-care blood work showed hyperlactatemia at 4.5 mmol/L, PCV/TS of 53%/7.8 g/dl, mild metabolic acidosis, normal electrolytes and renal values. The arterial blood pressure (Doppler) was at 130 mm Hg.
As the dog was getting flow-by oxygen, an abbreviated thoracic point-of-care ultrasound (T-POCUS) was performed (see below).
Continue reading “Pulmonary thromboembolism in dogs and cats: to lyse or not to lyse? “