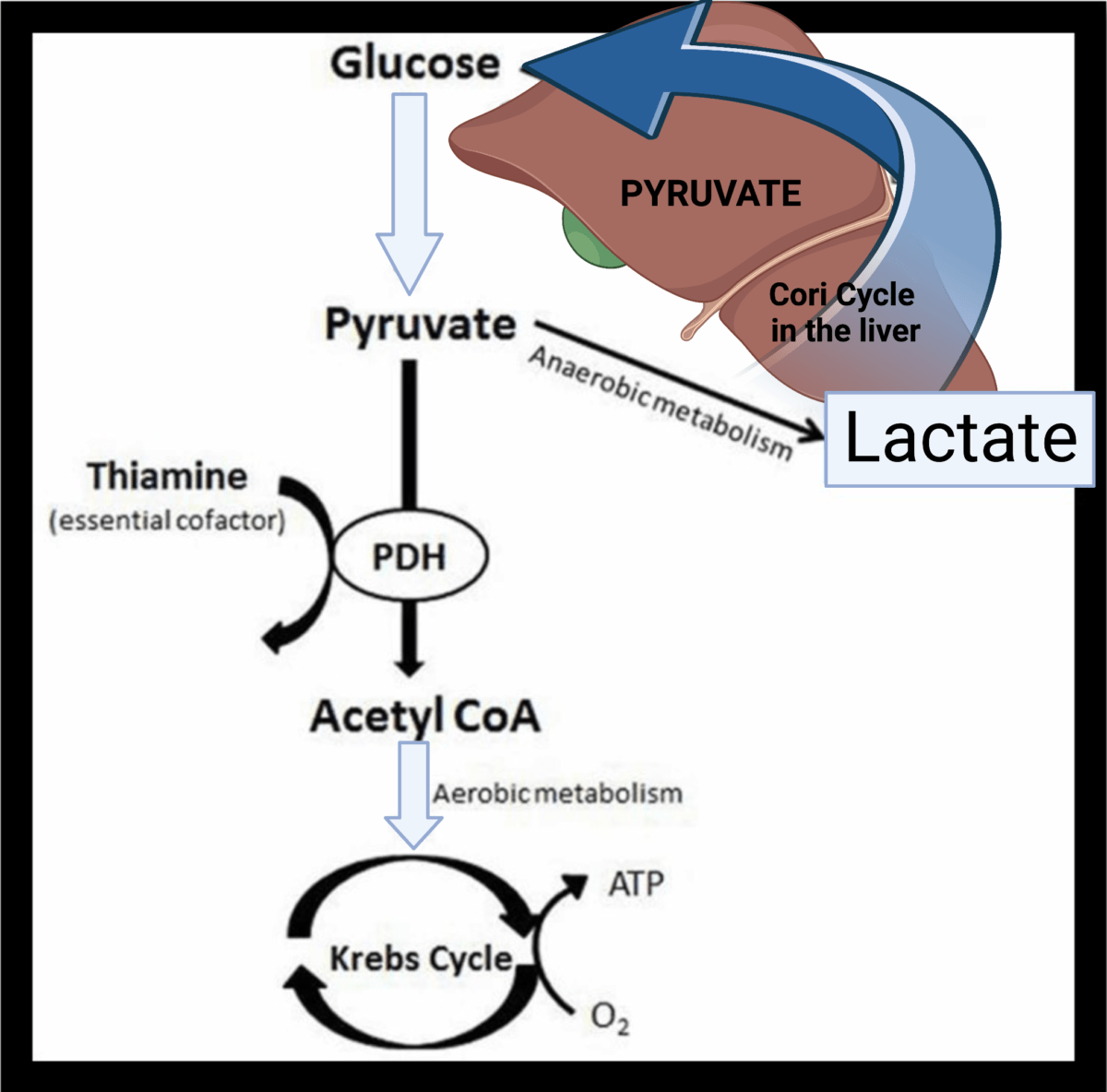
A lot of clinicians continue to believe that impaired tissue oxygenation is the main cause of increased blood lactate, and lactate itself results in metabolic acidosis. This biochemical understanding has persisted for long time, but there are some good reasons to challenge these traditional views on the ‘bad’ lactate.
After its production by anaerobic glycolysis lactate is re-used in the liver and the kidneys, and it may be converted back to glucose. The important point though is that lactate is also produced via aerobic glycolysis as a response to catecholamine release and stress. This may happen in septic patients, albuterol toxicity, trauma and other critical illnesses. In these clinical scenarios, the trigger for lactate production is adrenergic stimulation and not lack of oxygen.
If you want to learn more about lactate metabolism, watch this short video below: