A 3-year-old castrated male domestic shorthaired cat was presented to the emergency service for evaluation of acute severe lethargy, anorexia and vomiting. He has been strictly outdoors and was previously in good health. His last annual examination and blood work were performed 2 weeks ago, and they were within normal limits.
Today, his physical examination showed a body temperature of 97F (36.1C), heart rate of 140 beats per minute, respiratory rate of 44 breaths per minute, stuporous mentation, poor femoral pulses, pale pink mucous membranes, unkempt haircoat and dehydration of at least 7-8%. An ECG, venous blood gas, and thoracic/abdominal point-of-care ultrasound (POCUS) were performed during the primary survey as the intravenous catheter was being placed.
Venous blood gas results:
pH = 6.942 (Reference interval, 7.3-7.409)
pCO2 = 26.2 mm Hg (RI, 32.7-44.7)
BE(ecf) = -26.7 (RI, 0-6)
HCO3 = 5.71 mmol/L (RI, 18-23.2)
Na = 124.3 mmol/L (RI, 150.5-157.2)
K = 6.36 mmol/L (RI, 3.5-4.4)
Ionized Ca = 0.68 mmol/L (RI, 1.15-1.35)
Lactate = 1.2 mmol/L (RI, 0-2.5)
Glucose = 225 mg/dl (RI, 65-131)
ECG: Sinus bradycardia
POCUS: hyperdynamic left ventricle, small CVC, no pleural/pericardial/peritoneal effusion, normal lung ultrasound, small urinary bladder
Abbreviated chemistry panel:
Creatinine = 17.91 mg/dl = 1583 umol/L (RI, 0.8-1.6 mg/dl)
BUN = 423 mg/dl = 151 mmol/L (RI, 19-33 mg/dl)
Phosphorous = 23.3 mg/dl (RI, 3.8-7.5)
Total magnesium = 3.6 mg/dl (RI, 1.7-2.3)
Total calcium = 8.4 mg/dl (RI, 8.4-11.8)
Albumin = 2.8 g/dl = 28 g/L (RI, 2.5-3.3 g/dl)
Total bilirubin = 0.5 mg/dl (RI, 0-0.6)
ALT, ALKP, GGT = within normal limits
Hematocrit: 29%
Total protein: 8.1 g/dl = 81 g/L (RI, 6-8)
As you can see, this feline patient has numerous findings on physical examination and admission blood work that must be addressed during initial stabilization, however we will focus on his severe ionized hypocalcemia this time.
Calcium homeostasis is a complex process that involves five key components:
- Serum calcium
- Serum phosphate
- Calcitriol (active vitamin D, also known as 1,25-dihydroxyvitamin D3)
- Parathyroid hormone (PTH)
- Fibroblast growth factor 23 (FGF-23), a hormone that plays a pivotal role in phosphorus (directly) and calcium (indirectly) regulation.
These components regulate calcium metabolism, i.e., the movement of calcium in the gut, kidney, and bones. Calcium has to be consumed from the diet because animals and people can’t make this mineral. Therefore, the amount of calcium stored in the body largely depends on dietary intake, intestinal absorption, bone remodeling, and renal excretion. If an animal doesn’t eat enough calcium, the body will move calcium from bones to blood to maintain serum calcium levels at a constant level.
If we go back to our feline patient, it is quite obvious that the cat has developed severe acute kidney injury (AKI). What’s interesting is that AKI and chronic kidney disease (CKD) may lead to both ionized HYPO- and HYPERcalcemia.
In a cohort of 238 cats with HYPERcalcemia from a referral hospital population (Broughton et al. JVIM 2023), 13% of these cats had AKI and 8.4% of the cats were diagnosed with CKD. On the other hand, Coady et al. (Front Vet Sci 2019) described 450 cats with HYPOcalcemia. Kidney injury accounted for 21.6% of all cases of feline HYPOcalcemia, of which 62.9% (61/97 cats) were diagnosed with AKI and 37.1% (36/97) were diagnosed as CKD. Urethral obstruction accounted for 15.1% (68/450) of all cases.
In our critical feline patient presented above, the ionized calcium concentration was 0.68 mmol/L, which is considered very severe and may result in development of significant clinical signs (e.g. muscle tremors, facial rubbing, stiff gait, pyrexia, prolonged QT-interval, hypotension, and hypersensitivity to stimuli).
So, why would some animals with kidney injury develop LOW blood calcium concentration, while others develop HYPERcalcemia?
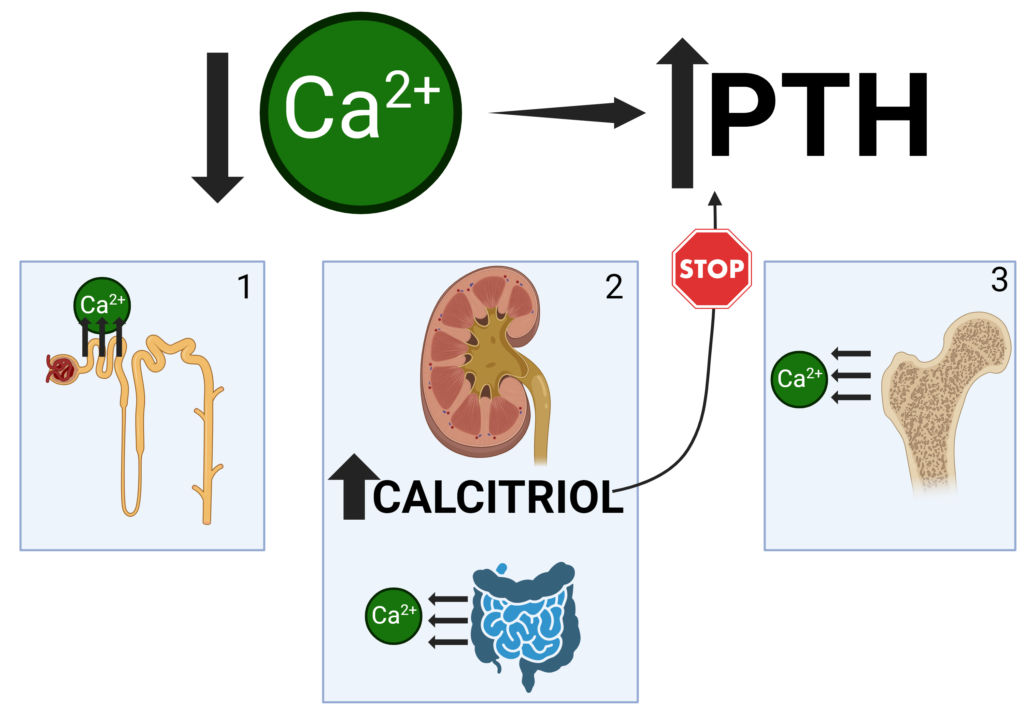
Calcium homeostasis
In health, a decrease in serum calcium causes the parathyroid gland to secrete more PTH hormone. PTH, in turn, will have 3 important effects on calcium homeostasis (Figure 1):
1) In the kidney: PTH will increase tubular calcium reabsorption
2) In the kidney: PTH will also increase calcitriol secretion ⇒ Calcitriol will lead to calcium reabsorption in the gut and will decrease PTH secretion in the parathyroid gland (negative feedback loop)
3) In bone: PTH will increase net bone resorption
In other words, low calcium ⇒ PTH secretion (+calcitriol secretion) ⇒ NET increase in blood calcium
What about AKI?
AKI causes an abrupt decrease in glomerular filtration rate (GFR) leading to accumulation of phosphorus in the blood (hyperphosphatemia) since glomerular filtration of phosphorus is an important mechanism of phosphorus excretion from the body. An increase in serum phosphate stimulates FGF-23 secretion from bone, which acts in proximal tubular cells of the kidney to decrease phosphate reabsorption resulting in NET EXCRETION of phosphate from the body (Figure 2):
In other words, AKI ⇒ high phosphate ⇒ FGF-23 secretion in bone ⇒ NET EXCRETION of phosphate to improve hyperphosphatemia.
On top of that, FGF-23 reduces renal secretion of calcitriol which decreases intestinal phosphate AND calcium absorption.
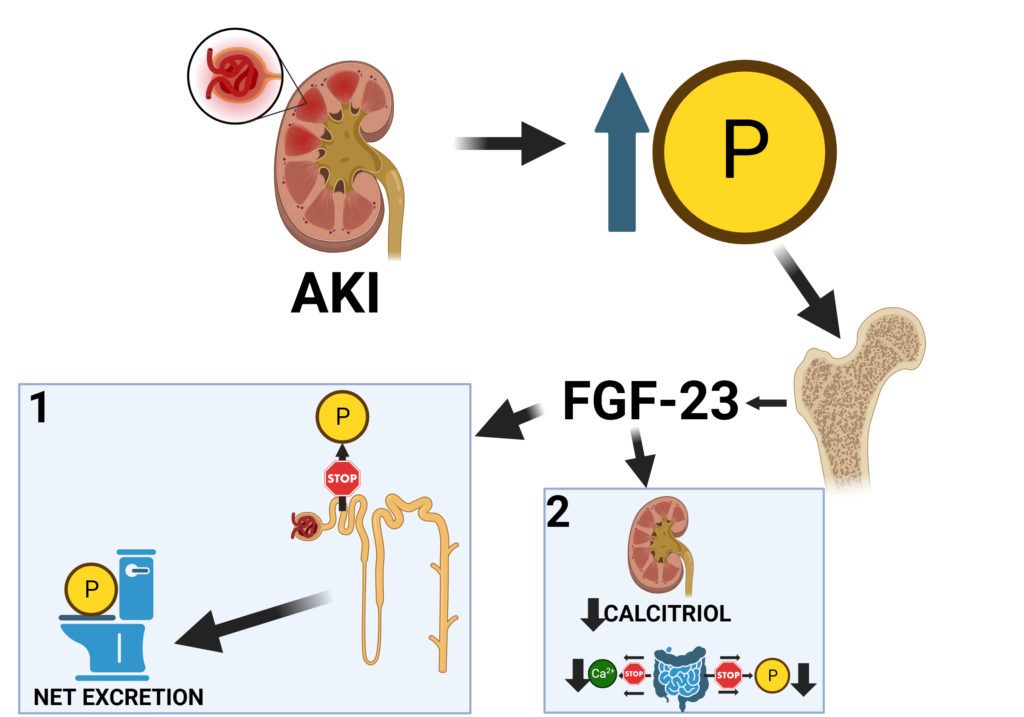
To a lesser extent, markedly increased serum phosphate concentration leads to mass law interactions with calcium that may result in decreased ionized calcium as well. From experimental research (Adler et al, Kidney International 1985), we know that to decrease iCa concentration by 0.1 mg/dl (~0.02 mmol/L), serum phosphate concentration must increase by 3.7 mg/dL.
In our feline case, serum phosphate went up from 5-7 mg/dl (upper reference range) to 23.3 mg/dL, which in theory may decrease iCa only by 0.1-0.12 mmol/L and can’t explain the drop of iCa from normal 1.2 to 0.68 mmol/L in this cat.
These complex interactions and pathophysiology behind the development of hypocalcemia secondary to AKI can be summarized in these two simple sentences:
- AKI causes hyperphosphatemia that promotes reduced calcitriol production (via FGF-23) in the kidneys leading to decreased serum calcium.
- In addition, AKI-induced hyperphosphatemia causes direct reduction in ionized calcium via physicochemical reaction.
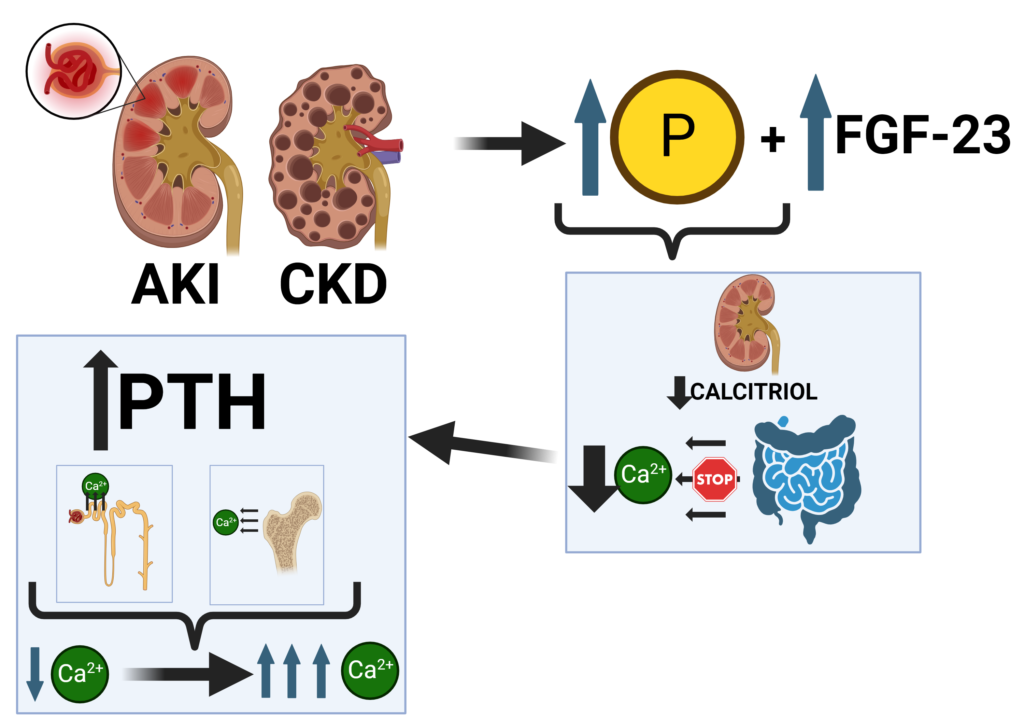
But why would some other patients present with HYPERcalcemia associated with AKI or CKD?
As renal function decreases in patients with AKI and CKD, increased phosphate retention results in a rise in serum phosphate and FGF-23 levels. Meanwhile, a reduction in calcium absorption caused by decreased calcitriol secretion leads to a fall in serum calcium and a rise in PTH. Chronic elevations of PTH (i.e. secondary and then tertiary hyperparathyroidism) result in increased tubular calcium reabsorption in the kidney and bone that will eventually lead to normalization of calcium levels followed by HYPERcalcemia (Figure 3).
In secondary hyperparathyroidism, the serum calcium is normal and the PTH level is elevated.
Tertiary hyperparathyroidism is characterized by excessive secretion of PTH after long-standing secondary hyperparathyroidism, in which hypercalcemia has ensued.
Are there any other causes of HYPERcalcemia in animals with AKI?
It is important to remember that canine patients with Addison’s disease may present with hypercalcemia and acute azotemia, however these two blood work abnormalities are likely minimally related to each other in this population of patients.
In addition, long-standing severe hypercalcemia (e.g. secondary to cholecalciferol toxicity) may cause AKI by itself. The reversible decrease in glomerular filtration rate in severe hypercalcemia is thought to be mediated in part by direct renal vasoconstriction. On top of that, volume depletion caused by vomiting and polyuria as well as renal tissue calcification may contribute to worsening of kidney function. A defect in urinary concentrating ability secondary to hypercalcemia is thought to be due to downregulation of aquaporin-2 water channels in the collecting tubules and tubulointerstitial injury caused by calcium deposition in the medulla (Rosen et al. Kidney int 1990; Earm J Am Soc Nephrol 1998).
Are there any other causes of HYPOcalcemia in animals with AKI?
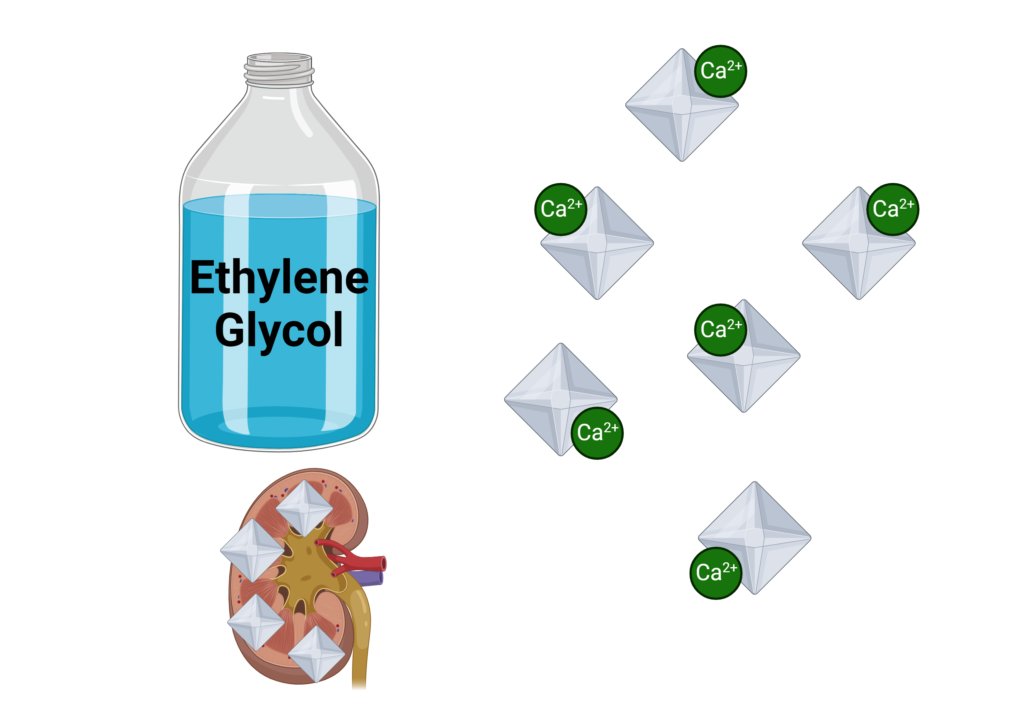
Another important consideration when dealing with severe ionized hypocalcemia in a feline or canine patient presenting with AKI is a possibility of ethylene glycol (EG) toxicity. It is a well-known fact that metabolites of EG can chelate calcium and become deposited in soft tissues including kidneys, resulting in severe hypocalcemia (Figure 4). Hypocalcemia often develops later when renal function is severely reduced from acute renal failure and when hyperphosphatemia is severe. As a side note, EG toxicity was our top differential in this strictly outdoor cat.
WOW! That’s a ton of pathophysiology compressed in one short blog post. I hope I didn’t overwhelm you. Although it might be cool to know all this information and impress your colleagues and friends, you may not need to know ALL of that in your clinical emergency practice.

However, I would take away the following bullet points from this conversation:
- Cats with AKI may have low, normal or high ionized calcium depending on the stage of the disease and other comorbidities.
- Hyperphosphatemia is the main pathophysiologic mechanism that is driving complex hormonal changes resulting in calcium derangements in this population of patients.
- Ethylene glycol toxicity should be highly suspected in outdoor animals presenting with severe AKI and ionized hypocalcemia.
- Marked ionized hypocalcemia (<0.7-0.85 mmol/L) may lead to severe clinical signs including arterial hypotension and ECG abnormalities, therefore it should be corrected as soon as possible.
References
Broughton SE, O’Neill DG, Syme HM, Geddes RF. Ionized hypercalcemia in 238 cats from a referral hospital population (2009-2019). J Vet Intern Med. 2023 Jan;37(1):80-91. doi: 10.1111/jvim.16627. Epub 2023 Jan 16. PMID: 36645022; PMCID: PMC9889682.
Coady M, Fletcher DJ, Goggs R. Severity of Ionized Hypercalcemia and Hypocalcemia Is Associated With Etiology in Dogs and Cats. Front Vet Sci. 2019 Aug 22;6:276. doi: 10.3389/fvets.2019.00276. PMID: 31508432; PMCID: PMC6714612.
Adler AJ, Ferran N, Berlyne GM. Effect of inorganic phosphate on serum ionized calcium concentration in vitro: a reassessment of the “trade-off hypothesis”. Kidney Int. 1985 Dec;28(6):932-5. doi: 10.1038/ki.1985.220. PMID: 4087699.
Rosen S, Greenfeld Z, Bernheim J, Rathaus M, Podjarny E, Brezis M. Hypercalcemic nephropathy: chronic disease with predominant medullary inner stripe injury. Kidney Int. 1990 Apr;37(4):1067-75. doi: 10.1038/ki.1990.87. PMID: 2342245.
Earm JH, Christensen BM, Frøkiaer J, Marples D, Han JS, Knepper MA, Nielsen S. Decreased aquaporin-2 expression and apical plasma membrane delivery in kidney collecting ducts of polyuric hypercalcemic rats. J Am Soc Nephrol. 1998 Dec;9(12):2181-93. doi: 10.1681/ASN.V9122181. PMID: 9848772.


Your writing style is captivating.
Fantastic read! I was especially impressed by the depth provided on the topic, offering a perspective I hadn’t considered. Your insight adds significant value to the conversation. For future articles, it would be fascinating to explore more to dive deeper into this subject. Could you also clarify more about the topic? It caught my interest, and I’d love to understand more about it. Keep up the excellent work!
I was suggested this web site by my cousin. I’m not sure whether this post is written by him as no one else know such detailed about my trouble. You are incredible! Thanks!
I appreciate your honesty in this post. It’s refreshing to see someone talk openly about the challenges of remote work. Check out Asian Drama for more real-life experiences.
You’re brilliant
BaddieHub This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
Hi i think that i saw you visited my web site thus i came to Return the favore I am attempting to find things to improve my web siteI suppose its ok to use some of your ideas
SocialMediaGirls You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Touch to Unlock I like the efforts you have put in this, regards for all the great content.