A 12-year-old female spayed Chihuahua was presented to the emergency service for evaluation of respiratory distress that had started acutely several hours prior to presentation. The dog began coughing at 10 am the morning of presentation, and was unobserved during the day while the owner was at work. At 6 pm the cough was worse, and the dog became dyspneic. The patient has had a chronic cough for a couple years but typically only has one coughing episode per day. The cough was a hacking cough that lasted about 10-15 seconds, and the dog has never been dyspneic before.
On admission to the emergency service, the patient had a moderate mixed dyspnea with respiratory rate of 60/min, heart rate of 130/min and body temperature of 99.5 F. There were diffuse crackles ausculted bilaterally as well as a II/VI left apical systolic murmur. Pulse quality, mucous membrane color and capillary refill time were within normal limits for a canine patient.
The dog received a single injection of furosemide at 2 mg/kg, butorphanol at 0.2 mg/kg and was placed in an oxygen cage (FiO2=0.6). Thoracic radiographs were taken within an hour of admission (Figure 1-3).



Thoracic radiographs showed moderate right-sided cardiomegaly with mild left atrial enlargement without evidence of pulmonary venous congestion; and moderate to marked diffuse mixed pulmonary pattern.
Based on these findings the top differential diagnoses included:
- Non-cardiogenic pulmonary edema secondary to pulmonary hypertension
- Negative pressure pulmonary edema secondary to upper airway obstruction/prolonged coughing episode
- Pulmonary hemorrhage
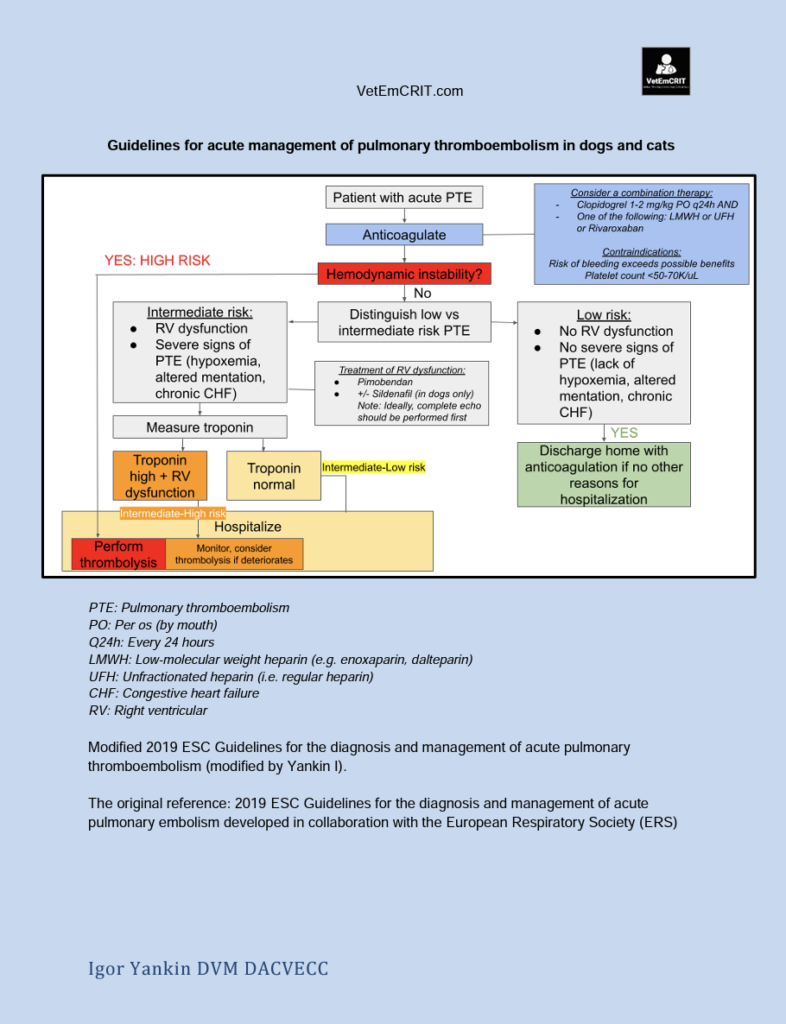
- Pulmonary thromboembolism
- ARDS
Within the next 8 hours the patient’s dyspnea did not improve and the following diagnostics were performed:
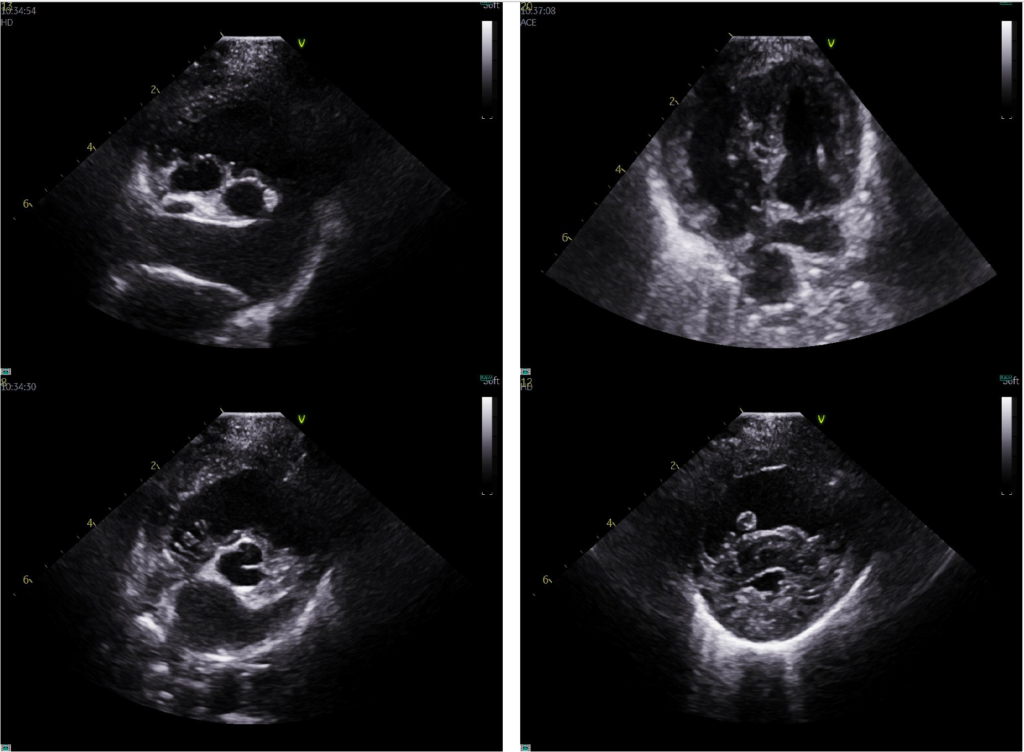
- Echocardiography (Figure 4)
- Venous blood gas, CBC, Chemistry: PCV/TS 61%/7.6, pH 7.33 (RR 7.38-7.49), lactate 4.8 (RR <2.5), leukocytosis (22.9 k/uL; RR 5k-16k) with mature neutrophilia (17.9k; RR 2.95k-11.64k) and adequate platelet count;
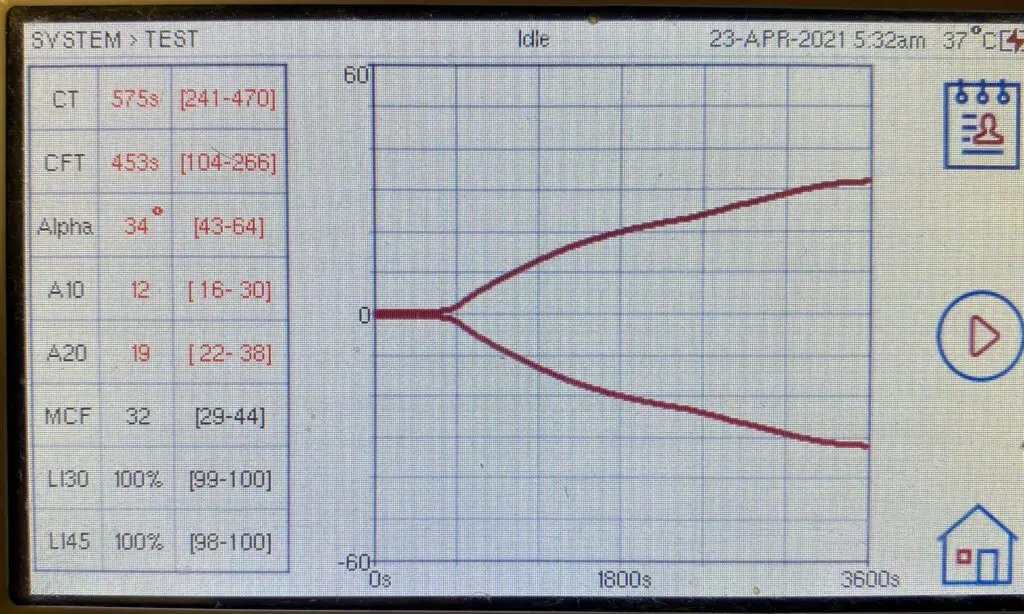
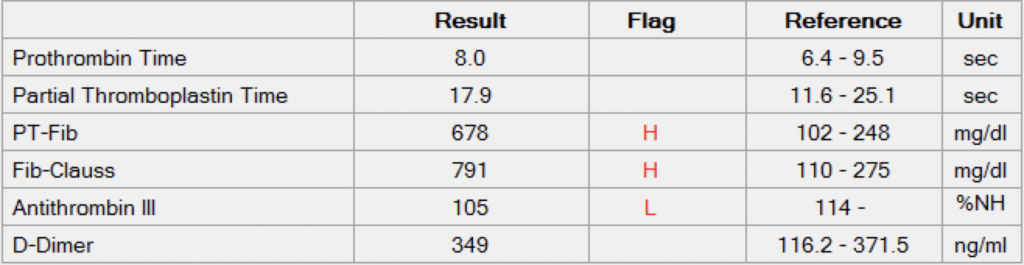
- Coagulation profile and viscoelastic testing (Figure 5 and 6)
- 4DX SNAP: Negative for heartworm antigen and Lyme, Borrelia, and Anaplasma antibodies
- Urinalysis: within normal limits
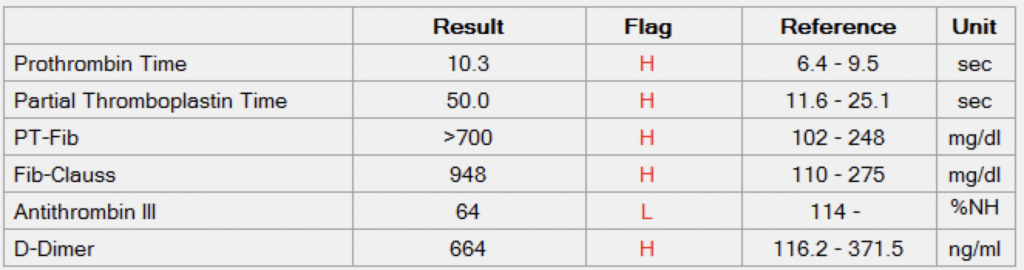
Based on these findings, the patient was started on sildenafil at 3 mg/kg by mouth every 8 hours and was continued on oxygen therapy (FiO2=0.4-0.6) for the next 48 hours. No additional treatments were performed. This therapy resulted in complete resolution of dyspnea and coagulopathy. Recheck coagulation panel, VCM and thoracic radiographs are depicted below (Figure 7-9).



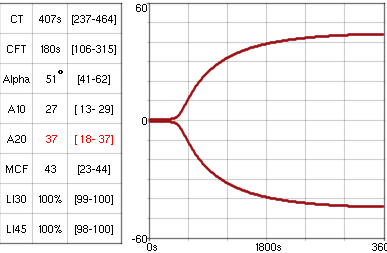
Figure 8. Resolved coagulopathy 48 hours after presentation and treatment with sildenafil/oxygen: Normalized PT, PTT and changes on VCM.
Dynamic intrathoracic tracheal (moderate) and mainstem bronchial (severe) narrowing, secondary to chondromalacia; unchanged left atrial and right sided cardiomegaly.
Case Discussion
The described-above canine patient was diagnosed with severe pulmonary hypertension (PH) and transient coagulopathy along with pulmonary infiltrates that resolved within 48 hours after commencement of sildenafil and oxygen therapy. Both PH-induced lung infiltrates as well as hypocoagulability are rare phenomena not commonly reported in human and veterinary literature.
Pulmonary alveolar infiltrates associated with pulmonary hypertension have been described by Kellihan et al. 2015 in 10 canine patients. Similar to our patient, none of the dogs reported by Kellihan had evidence of significant left-sided heart disease or pneumonia. Non-cardiogenic pulmonary edema induced by upper airway obstruction or prolonged coughing (aka negative pressure pulmonary edema) was another important differential in our canine patient, especially considering the fact that mainstem bronchial and tracheal collapse were confirmed via fluoroscopy. In Kellihan et al. paper, authors speculated about the proposed mechanisms explaining the development of pulmonary infiltrates in patients with severe PH:
“Specifically, we hypothesize that patchy edema in our patients is caused by non-uniformity in pulmonary capillary perfusion in which some capillary beds are over-perfused relative to others. An analogous mechanism is the development of high altitude pulmonary edema (HAPE) in humans with acute, hypoxia-induced PH. The capillaries in the poorly constricted region experience higher hydrostatic pressure and alveolar membrane integrity is compromised, resulting in edema formation with high protein and high red blood cell composition. Patchy pulmonary alveolar infiltrates in the dogs with moderate to severe PH, may also be arising as a result of focal over-perfusion of select capillary beds, comparable to HAPE. The reduction of infiltrates by sildenafil suggests that it may reduce perfusion heterogeneity, thereby relieving the hydrostatic pressure in over-circulated areas”.
Similarly, an acute negative pressure pulmonary edema may improve over time, and it is unlikely that we will be able to definitively differentiate PH-induced pulmonary infiltrates from negative pressure pulmonary edema in our patient.
The transient coagulopathy diagnosed via a coagulation profile and viscoelasting testing was another interesting finding that is worth our discussion. To the best of my knowledge, PH-associated coagulopathy resolving 48 hours after initiation of sildenafil has never been reported in veterinary medicine, but was described in human medical literature. Vrigkou et al. 2020 studied 44 new human patients with pulmonary arterial hypertension (22 with idiopathic PAH and 22 with connective tissue disease) and 25 healthy controls. In that study, PAH patients were shown to have:
(1) diminished platelet aggregation
(2) unstable platelet aggregate formation
(3) impaired initiation of the clotting process and clot propagation
(4) defective thrombin formation capacity
(5) normal final clot firmness
(6) accelerated rate of clot lysis.
Vrigkou et al. 2020: “These findings portray a complex impairment of the hemostatic processes in the PAH setting. Primary hemostasis appears to be defective in that population, as shown by the decreased percentage of platelet aggregation and the presence of disaggregation in LTA testing. Secondary hemostasis is, also, impaired as suggested by the ROTEM results. The prolonged CT parameter of the ROTEM assay reflects the decreased rate of fibrin formation, which is dependent on thrombin formation”.
Similar to Vrigkou’s findings, our canine patient had prolonged CT and CFT documenting impaired initiation of the clotting process and clot propagation, whereas final clot firmness remained preserved.
Vrigkou et al. 2020: “Pulmonary arterial hypertension is a chronic and progressive disorder, where endothelial dysfunction plays a central role in its development and evolution. The chronic injury to the pulmonary endothelium could result in chronic platelet and coagulation cascade activation, extended platelet degranulation and, subsequently, in platelet function abnormalities. The chronic activation of the patients’ procoagulant pathways could lead to the exhaustion of coagulation factors and, consequently, to their diminished hemostatic capacity. Thus, our findings of decreased platelet aggregation, disaggregation, prolonged CT and CFT values, reduced thrombin generation capacity and increased levels of markers of platelet activation are consistent with that theory. The elevated D-dimer levels and the mild prolongation of the INR and aPTT parameters could also reflect the prolonged activation of the coagulation processes”.
The Bottom Line
Emergency veterinarians should be aware of PH-associated pulmonary infiltrates and hypocoagulability that may resolve after initiation of sildenafil therapy and supportive care.
References
Vrigkou E, Tsantes AE, Kopterides P, Orfanos SE, Armaganidis A, Maratou E, Rapti E, Pappas A, Tsantes AG, Tsangaris I. Coagulation Profiles of Pulmonary Arterial Hypertension Patients, Assessed by Non-Conventional Hemostatic Tests and Markers of Platelet Activation and Endothelial Dysfunction. Diagnostics (Basel). 2020 Sep 27;10(10):758. doi: 10.3390/diagnostics10100758. PMID: 32992591; PMCID: PMC7601126.
Kellihan HB, Waller KR, Pinkos A, Steinberg H, Bates ML. Acute resolution of pulmonary alveolar infiltrates in 10 dogs with pulmonary hypertension treated with sildenafil citrate: 2005-2014. J Vet Cardiol. 2015 Sep;17(3):182-91. doi: 10.1016/j.jvc.2015.04.002. Epub 2015 Aug 17. PMID: 26293206.
Vrigkou E, Tsangaris I, Bonovas S, Kopterides P, Kyriakou E, Konstantonis D, Pappas A, Anthi A, Gialeraki A, Orfanos SE, Armaganidis A, Tsantes A. Platelet and coagulation disorders in newly diagnosed patients with pulmonary arterial hypertension. Platelets. 2019;30(5):646-651. doi: 10.1080/09537104.2018.1499890. Epub 2018 Jul 26. PMID: 30047809.


Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Your article helped me a lot, is there any more related content? Thanks!
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?