Acid-base analysis in a cat can be deceptively complex, especially when traditional parameters like pH, pCO₂, and bicarbonate appear normal. In this case, advanced analysis revealed a hidden mixed disorder that would have been missed without deeper evaluation.
You are presented with a 12-year-old spayed female domestic shorthair cat with a history of injection-site sarcoma and diabetes mellitus. She is currently being treated with an SGLT2 inhibitor, a sodium–glucose co-transporter-2 blocker.
On physical examination, she was dull, dehydrated, and hypothermic.
A venous blood sample was obtained immediately after IV catheter placement. The collection was performed under strict anaerobic conditions, without struggling, and with no evidence of sampling error.
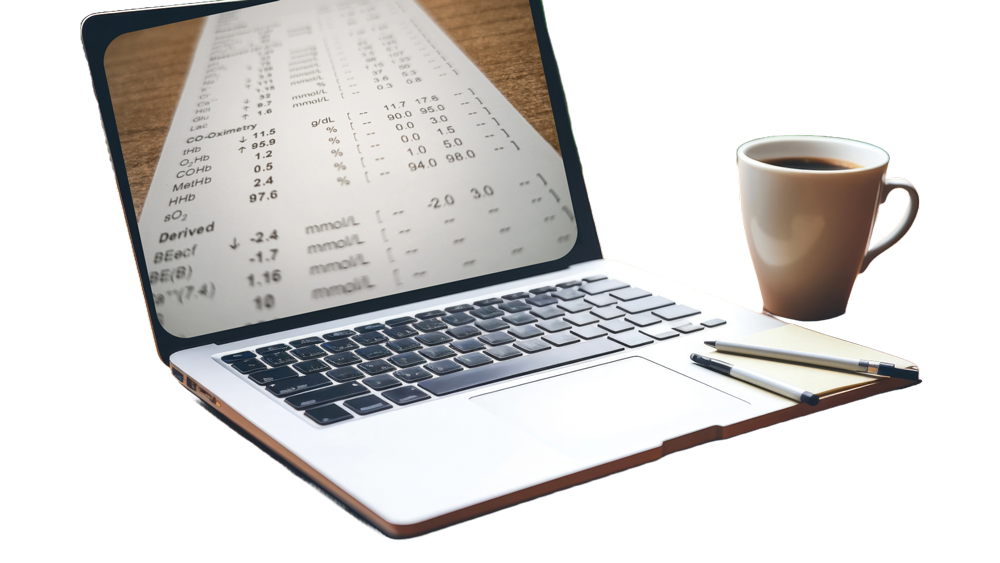
The venous blood gas panel was then analyzed, and the results are shown below.
- pH = 7.427 (Reference: 7.244 – 7.444)
- pCO₂ = 28.7 mmHg (Reference: 27.3 – 49.1)
- HCO₃⁻ = 19.11 mmol/L (Reference: 15.9 – 24.7; mid-normal: )
- Base excess (BEecf) = – 5.5 mmol/L (Reference: -10.4 to -0.5)
- Sodium = 137.4 mmol/L (Reference: 150.5 – 157.2; mid-value: 153.9)
- Potassium = 2.96 mmol/L (Reference: 3.11 – 4.64)
- Chloride = 95.9 mmol/L (Reference: 113 – 123; mid-value: 118)
- Ionized calcium = 1.15 mmol/L (Reference: 1.21 – 1.45)
- Glucose = 135 mg/dL, or 7.5 mmol/L (Reference: 74 – 159 mg/dL = 4.1 – 8.8 mmol/L)
- Lactate = 2.3 mmol/L (Reference: 0 – 3.3 mmol/L)
- Creatinine = 1.25 mg/dL, or 110.5 µmol/L (Reference: 0.8 – 1.8 mg/dL = 70.7 – 159.1 µmol/L)
- BUN = 20 mg/dL, or 7.1 mmol/L (Reference: 19 – 33 mg/dL = 6.8 – 11.8 mmol/L mmol/L)
- Anion gap = 25.4 (Reference: 14.8 – 23.8; mid-normal: )
- Albumin = 3.5 g/dL = 35 g/L (Reference: 2.2 – 4 mg/dL; mid-normal value: 3.1 mg/dL)
- Phosphate = 1.3 mmol/L = 3.9 mg/dL (Reference: 3.1 – 7.5 mg/dL; mid-normal value: 5.3 mg/dL)
Now, let’s apply the advanced traditional approach to this case to perform an acid-base analysis in this cat.
Step-by-step acid-base analysis in a cat
Step 1: Get Labs and Determine Sample Type
First, we confirm the sample type—it’s venous blood—and we are using the appropriate venous reference intervals.
Step 2: Verify Sample Quality
There was no reported concern regarding sample collection, such as air exposure, excessive delay, or struggling.
So we can proceed with interpretation.
Step 3: Look at the pH
The pH is 7.427, which is within the reference range.
According to the traditional approach, this suggests that there is either no acid-base abnormalities, or there is a mixed disorder since full compensation is very rare.
Step 4: Evaluate pCO₂
The pCO₂ is 28.7 mmHg, which is within the normal reference range.
Thus, there is no obvious primary respiratory abnormality based on pCO₂ alone.
Step 5: Evaluate HCO₃⁻ and/or Base Excess
The bicarbonate (HCO₃⁻) is 19.11 mmol/L and the base excess is -5.5 mmol/l, which are also within the normal reference range for cats.
At this point, using the traditional basic analysis, we would typically conclude that no obvious acid-base disorder is present, since pH, pCO₂, and HCO₃⁻ are all in the normal range.
However, now we will proceed to the additional advanced steps that I recommend performing in all cases.
Step 6: Calculate the Anion Gap
In the traditional textbook approach, anion gap isn’t usually calculated unless there’s clear evidence of metabolic acidosis based on the first five steps.
However, I recommend calculating the anion gap in all cases, regardless of the pH, bicarbonate, or pCO₂.
That’s because you can have a combined high anion gap metabolic acidosis and metabolic alkalosis — and the opposing effects may cancel each other out, resulting in a normal-looking pH that could be misinterpreted as a normal acid-base status.
The veterinary formula for anion gap (AG) is the sum of sodium and potassium minus the sum of chloride and bicarbonate.
AG = (Na + K) – (Cl + HCO₃)
Once we plug in all values, the anion gap is going to end up being:
AG = (137.4 + 2.96) – (95.9 + 19.11) = 25.4
AG = 25.4 mEq/L
The feline reference interval for anion gap is around 14.8 – 23.8 mEq/L, therefore our patient’s anion gap is elevated at 25.4 mEq/L, suggesting the presence of unmeasured anions.
Step 7: Correct the Anion Gap for Hypoalbuminemia (Albumin-Adjusted AG)
Since this cat’s albumin level is 3.5 g/dL, or 35 g/L, and it falls within the normal reference range, we’ll skip this step—there’s no need to correct the anion gap for hypoalbuminemia.
However, in patients with significantly low albumin, correcting the anion gap may reveal an elevated value that was initially masked.
Step 8: Calculate the Delta/Delta Ratio
Since this cat’s anion gap is elevated, we can now calculate the delta/delta ratio to check for a hidden mixed acid–base disorder.
To do this, we divide the change in anion gap by the change in bicarbonate using the following formula:
Delta/delta = (Patient’s AG – Mid-normal AG) ÷ (Mid-normal HCO₃⁻ – Patient’s HCO₃⁻)
Let’s plug in the values:
- Mid-normal anion gap = 19.3 mEq/L
- Mid-normal bicarbonate = 20.3 mmol/L
- Patient’s anion gap = 25.4
- Patient’s bicarbonate = 19.11
So:
Delta/delta = (25.4 – 19.3) ÷ (20.3 – 19.11)
= 6.1 ÷ 1.19
= 5.1
A delta/delta ratio above 2 suggests that the rise in anion gap is out of proportion to the drop in bicarbonate— This means there’s a concurrent metabolic alkalosis occurring alongside a high anion gap metabolic acidosis.
In other words, this cat is hiding a mixed acid–base disorder—something that would have been missed if we had only looked at the pH, pCO₂, and bicarbonate, which all appeared normal in the traditional textbook approach.
Step 9: Final Interpretation of the Acid–Base Status and Differential Diagnoses
Let’s wrap it all up.
Based on the advanced traditional analysis, this cat has a mixed acid–base disorder with two opposing components:
- A high anion gap metabolic acidosis was identified based on the elevated anion gap of 25.4 mEq/L, and
- A concurrent metabolic alkalosis that’s nearly equal in magnitude was revealed by the disproportionately high delta/delta ratio of 5.1.
These two forces essentially cancel each other out, which explains why the pH, bicarbonate, and pCO₂ all appeared normal at first glance.
Given the cat’s history and physical examination, the most plausible differential for the high anion gap metabolic acidosis was ketoacidosis, that was confirmed by a beta-hydroxybutirate blood level of 4 mmol/L, consistent with diabetic ketoacidosis.
The cat’s history of SGLT2 inhibitor use supports the diagnosis of euglycemic DKA—a form of DKA that occurs even with normal blood glucose.
Lactate was within normal range at 2.3 mmol/L, but it was likely slightly contributing to the elevated anion gap.
The concurrent metabolic alkalosis was most likely due to severe chloride depletion caused by vomiting, as reported in the history, and possibly functional ileus induced by pancreatitis that were confirmed on abdominal ultrasound.
So, in this case, the cat was diagnosed with a complex mixed acid–base disorder consisting of:
- Euglycemic diabetic ketoacidosis
- And a severe metabolic alkalosis due to gastric chloride loss and GI dysfunction
And none of this would have been detected if we had stopped after the basic traditional steps.
Despite a normal pH, normal pCO₂, and normal bicarbonate, this cat had a clinically significant acid–base disturbance that required deeper investigation.
This is exactly why adding these advanced steps—like calculating the anion gap, even when pH and bicarbonate are normal, and using the delta/delta ratio—can make a big difference in identifying hidden mixed disorders when performing acid-base analysis in a cat.
Author: Igor Yankin
Igor is the founder of VetEmCrit.com and a board-certified specialist in veterinary emergency and critical care. View all posts by Igor Yankin