This post presents diagnostic and therapeutic approaches to canine and feline patients with hyponatremia. As we all remember, the plasma sodium concentration represents a ratio of plasma sodium content to the water content. As a result, the plasma sodium concentration depends heavily on water balance. Therefore, hyponatremia may develop secondary to either excess of free water in the body or lack of sodium ions relatively to the free water. Also, it is helpful to remember that plasma sodium concentration is the key determinant of plasma osmolality, and the majority of hyponatremic patients will have low plasma osmolality. However, this is not always the case. For example, patients with hyperglycemia or those who received mannitol may develop hyponatremia in conjunction with high plasma osmolality caused by excessive glucose concentration or the presence of other osmotically active substances (e.g. mannitol). Hyponatremic patients with normal plasma osmolality typically have spurious hyponatremia (aka pseudohyponatremia).
Diagnostic approach
Step 1: Rule out hyponatremia with normal plasma osmolality
- Ideally, plasma osmolality should be measured as the first step to rule out hyponatremia with normal plasma osmolality (pseudohyponatremia);
- Since pseudohyponatremia occurs only if flame photometry analyzers are used (both modern blood gas analyzers (e.g. NOVA) and the majority of chemistry analyzers use a different technology), this step may be not relevant.
Step 2: Rule out hyponatremia with high plasma osmolality (translocational)
- The next step is to rule out hyperosmolar (translocational) hyponatremia (ideally, it is diagnosed via plasma osmolality measurement, however it is not always practical); the most common causes of hyperosmolar hyponatremia include hyperglycemia or hyperosmolar therapy/intoxication;
- If your patient is hyperglycemic, calculate the contribution of hyperglycemia to hyponatremia by using this formula:
- Expected decrement in Na+ in translocational hyponatremia = 2 x [(Current blood glucose in mg/dl – normal blood glucose in mg/dl)/100]
- If the expected decrement in Na+ does not fully explain the degree of hyponatremia, there should be another cause of hyponatremia aside from hyperglycemia;
- Next, review the patient’s medication history. If the patient received any hyperosmolar agents (e.g. mannitol, contrast substances), the hyponatremia should get corrected once this substance is eliminated from the patient’s system.
- If hyponatremia with normal and high plasma osmolarity is ruled out (see above), go to the step 3 – Hypoosmolar hyponatremia (the most common).
Step 3: Collect history and perform a physical examination to assess for various causes of hypoosmolar hyponatremia
3.1 Collect a thorough history, don’t forget to ask the following questions:
- Is the patient PU/PD?
- What medications your patient is on? Is the patient receiving IV fluids, tube feedings, diuretics?
- Has the patient been diagnosed with other comorbidities (especially, renal/cardiac/hepatic/thyroid conditions as well as hyper- or hypoadrenocorticism)?
- Are there any GI signs present?
3.2 Perform a full physical examination and point-of-care ultrasound to determine the volume status (not always possible and further diagnostics may be required – see step 3)
3.2.1 Patient is hypervolemic (=patient has gained both free water and sodium, but the gain of free water exceeded the gain of sodium leading to hyponatremia)
- Common findings on physical examination (PE): normal or high arterial blood pressure, chemosis (edematous conjunctiva), distended jugular veins, peripheral edema, body cavitary effusions, heart murmur (warning: effusions may be present in hypovolemic/normovolemic patients as well);
- Common causes of hypervolemic hyponatremia
- CHF
- AKI or advanced CKD; nephrotic syndrome
- Severe liver disease
- When hypervolemic hyponatremia occurs with cardiac failure or cirrhosis, the patient has advanced and, therefore, readily diagnosed disease.
3.2.2 Patient is hypovolemic (=patient has lost both free water and sodium, but the loss of sodium was in excess of free water)
- Common findings: A history of vomiting, diarrhea, diuretic use, diabetes mellitus (osmotic diuresis), along with increased thirst, dehydration, hypoperfusion (elevated heart rate, fair/poor femoral pulses, arterial hypotension, etc.);
- Common causes of hypovolemic hyponatremia:
- Renal losses (diuretics, Addison’s, kidney disease)
- Non-renal losses (GI, 3rd spacing secondary to pancreatitis, peritonitis, pleural effusion, uroabdomen, etc);
3.2.3 Patient is normovolemic (=patient has gained only free water resulting in dilution of plasma sodium concentration)
- No evidence of hypo- or hypervolemia on PE, however a completely normal examination cannot rule out occult hypovolemia/hypervolemia;
- Common causes of normovolemic hyponatremia:
- Psychogenic polydipsia, hypotonic fluid administration
- Hypothyroidism, myxedema coma
- SIADH
- Medications associated with SIADH:
- Chlorpropamide, Cyclophosphamide, Morphine, Barbiturates, Vincristine, Carbamazepine (Tegretol), Acetaminophen, NSAIDs, Antipsychotics, Antidepressants.
Step 4: Calculate fractional excretion of sodium (FENa) +/- urine and plasma osmolality measurements if the cause of hyponatremia is not apparent from the history and physical examination alone; this supplemental testing can also be performed to confirm your tentative diagnosis;
4.1 FENa = (Na+ urine/creatinine urine)/ (Na+ plasma/creatinine plasma) ×100
FENa < 1% (in the absence of diuretic therapy and osmotic diuresis) is suggestive of a non-osmotic stimulation of ADH caused by reduced effective circulating volume (i.e. low cardiac output state, arterial vasodilation, occult hypovolemia due to GI losses, hemorrhage, cavitary effusions, etc.)
- Look for any causes of occult hypovolemia and decreased cardiac output by performing a thorough physical examination, point-of-care ultrasound, echocardiography (cardiogenic, hypovolemic, obstructive, distributive causes);
- Address the cause of low cardiac output state (e.g. give isotonic to patient’s plasma fluid bolus if occult hypovolemia is suspected (see treatment guidelines below); vasopressors in vasodilatory state; positive inotropes in forward heart failure);
- If FENa <1% in the face of azotemia, this is likely prerenal azotemia;
- In the absence of diuretics, FENa should be below 1.0% in hyponatremic cardiac or cirrhotic patients, as the kidney function is normal and responding to decreased arterial perfusion in these edematous disorders.
FENa >1%: Differentials include acute kidney injury with tubular dysfunction or advanced chronic kidney disease, diuretic use, Addison’s disease
- Test for Addison’s (baseline cortisol to rule it out if it’s >2 OR ACTH stimulation test);
- In the absence of diuretics, AKI/CKD, Addison’s; go to the next step – 4.2
If FENa >1% + no history of diuretics, renal failure or osmotic diuresis, Addison’s disease + no evidence of hypoperfusion/hypovolemia ==> there is no physiologic stimulation of ADH and it is likely normovolemic hyponatremia (see 2.2.3).
- Rule out hypothyroidism (TTH + TT4);
- Rule out psychogenic polydipsia (history +/- measure daily water intake at home +/- water deprivation test if needed);
- Comparison of urine and plasma osmolality will be the best way to differentiate between psychogenic polydipsia (or hypotonic IV fluid administration) and SIADH;
- A urine osmolality > 100 mOsm/kg should be considered abnormal in a patient with hyponatremia and plasma hypoosmolality (suggestive of SIADH, given that other causes of hyponatremia ruled out by this time: no evidence of hypovolemia or low cardiac output, no evidence of cavitary effusions or edema, normal renal, hepatic, thyroid and adrenal functions, FENa >1%)
- A urine osmolality < 100 mOsm/kg would normally be expected as a result of complete suppression of ADH release (in psychogenic polydipsia).
- If mentioned-above conditions are ruled out, SIADH should be suspected
- Search for causes of SIADH:
- Medication history (see 2.2.3)
- Recent anesthesia/surgery (physical stress ==> ADH release)
- Search for pulmonary or central nervous system infections, vascular, or neoplastic diseases should reveal the cause in
Therapeutic approach
General concepts:
- The correct treatment of hyponatremia in acute illness depends first and foremost on the correct diagnosis! The only exception is the patient with acute symptomatic (i.e. presence of neurologic signs) hyponatremia that may be approached similar across various causes of hyponatremia during initial stabilization;
- Chronic hyponatremia (developed >24-48 hours ago) should be corrected not faster than 10-12 mmol/l per 24 hours to prevent osmotic demyelination; these patients demonstrate improved neurological symptoms initially, but one to several days later, new and progressive neurological symptoms emerge and can lead to permanent neurological deficits or even death;
- The change over 24 hour period is more important than per hour Na+ change;
- Majority of hyponatremic patients with moderate to severe hyponatremia will require a sampling line to monitor their plasma Na+ concentration every 4-6 hours;
- Acute symptomatic hyponatremia (very rare in veterinary medicine)
- In this situation sodium concentration dropped very acutely (over less than 24-36 hours) and the patient exhibits clinical signs consistent with cerebral edema (decreased mental status, seizures, tremors, other neurologic signs)
- This is the only situation when hyponatremia may be corrected as quickly as it occurred in the first place; delay in treatment of acute cerebral edema secondary to acute hyponatremia may lead to death;
- Consider giving 1 ml/kg of 3% hypertonic saline over 1 hour; this should increase serum Na+ by 2 mmol/l; if patient is very unstable from the neurologic stand point secondary to suspected cerebral edema, the dose and rate of administration may be increased;
- Serum Na+ can be measured after this infusion, and depending on its concentration and improvement in neurologic status, a decision to repeat hypertonic boluses can be made;
- If the patient with acute symptomatic hyponatremia has a hypervolemic phenotype (i.e. secondary to CHF, liver cirrhosis or renal failure) and this patient does not tolerate volume expansion, furosemide may be administered simultaneously to eliminate hypotonic urine;
- Once clinical signs attributed to acute hyponatremia has resolved, this patient may be approached as a patient with chronic hyponatremia – see step 2).
- Treatment of chronic hyponatremia (developed >24-48 hours ago or unknown onset) will vary in patients with hypervolemic, hypovolemic and normovolemic hyponatremia – see below.
2.1 Hypovolemic hyponatremia (see diagnostic guidelines above)
2.1.1 Correct hypovolemia by giving a bolus of fluids with fluid Na+ concentration similar to patient’s plasma Na+ concentration (+/- 5 mmol/L)
- In the majority of cases, a custom hypotonic solution should be made by either adding hypertonic saline to sterile water or adding sterile water to normal saline or other replacement solutions;
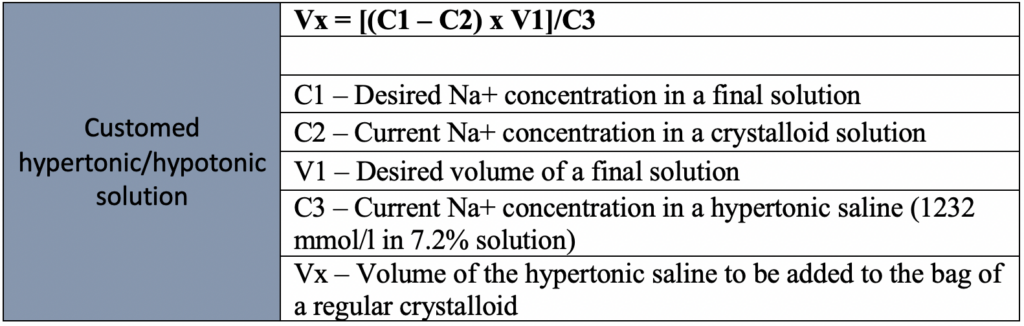
- The formula depicted below can be used to calculate how much hypertonic saline can be added to any baseline crystalloid solution in order to make a custom-made solution;
2.1.2 Correct dehydration + account for ongoing losses and maintenance requirements using the same custom-made solution with q4h plasma Na+ monitoring
Correction of hypovolemia and dehydration will eliminate ADH release and will correct hyponatremia;
Your main goal is to prevent correction of hyponatremia too rapidly (faster than 12 mmol/l per 24 hours) by manipulating fluid administration rate and its tonicity (e.g. if hyponatremia is getting corrected too fast, you can drop fluid sodium content even more; if hyponatremia is not getting corrected, make sure there are no other causes of hyponatremia (e.g. SIADH, Addison’s, etc) and consider increasing Na+ content of the IV fluids);
Comparison of urine and plasma osmolality may help to determine if there is an ongoing ADH release (appropriate for uncorrected hypovolemia or inappropriate)
- Patients with ongoing ADH release will have urine osmolality greater than plasma osmolality (because ADH will cause reabsorption of free water ==> will increase urine concentration);
- Patients with completely suppressed ADH release will have urine osmolality < plasma osmolality (usually <100-200 mosm/kg);
2.2 Hypervolemic hyponatremia
2.2.1 Secondary to heart failure/severe cardiac disease
- There is no specific treatment available other than augmentation of cardiac disease (e.g. with positive inotropes)
- Consider changing diuretic therapy:
- Although loop diuretics are more potent than thiazide diuretics, the latter are much more likely to cause hyponatremia. In one review of the literature on diuretic-induced hyponatremia (Spital et al. 1999), 73% was caused by thiazide diuretics alone, 20% by thiazide diuretics in combination with antikaliuretic agents, and only 8% due to furosemide alone; because thiazides block the sodium cotransporter in the renal cortex, only urinary dilution is disturbed. In contrast, loop diuretics such as furosemide block the NaK2Cl cotransporter in the medullary loop of Henle, and therefore, both urinary concentration and diluting mechanisms are impaired. As previously mentioned, furosemide may cause hypotonic urine and is thus much less likely to cause hyponatremia;
- Vaptans (ADH receptors antagonists) have been used in people, however they are very expensive, not readily available, and may provide very rapid correction;
- Another consideration is the patient’s appetite; if the patient with an advanced CHF does not eat well, it has limited ability to excrete electrolyte-free urine because the maximum urinary dilution is about 50 mmol/L; thus, to effectively excrete free water, one needs to consume enough solutes with food; This is the problem that causes hyponatremia with beer drinkers who are not eating. Beer is very hypotonic and contains little solute; therefore, these beer drinkers may develop hyponatremia with an intake of 6–10 l of beer/day. Normal solute intake in people is 600–800 mmol/day, thus allowing for substantial electrolyte free water excretion;
- Hyponatremia in CHF is a poor prognostic indicator of advanced heart disease;
2.2.2 Secondary to renal failure
- Hyponatremia in renal disease patients may be multifactorial: inability to excrete free water (hypervolemic hyponatremic patients), severe renal fluid losses (hypovolemic hyponatremia), iatrogenic hypotonic fluid administration via feeding tubes or IV route, or any combination thereof;
- If there are any concerns that the patient may be hypovolemic, this hypovolemia should be corrected (see guidelines for hypovolemic hyponatremia);
- If hyponatremia does not improve, this is likely due to renal inability to excrete free water +/- iatrogenic hypotonic fluid administration;
- Make sure this patient doesn’t receive excessive fluid administration;
- Consider hemodialysis if the patient is fluid overloaded and has inadequate urine production;
- Consider furosemide test if dialysis is unavailable or cannot be performed at the moment AND patient is hypervolemic on your examination;
2.3 Normovolemic hyponatremia (SIADH, psychogenic polydipsia or hypothyroidism)
- Psychogenic polydipsia: water restriction + addressing underlying cause;
- Hypothyroidism: hormonal replacement + consider water restriction if necessary;
- SIADH: try to identify an underlying cause and address it (see diagnosis guidelines) + water restriction (the main treatment) +/- furosemide;
- Classic sign of SIADH is worsening hyponatremia despite administration of IV fluids with high sodium content (e.g. NaCl 0.9%); this happens because collecting ducts continue to reabsorb free water from the administered IV solution but renal tubules are dumping sodium since there is normal circulating intravascular volume and no aldosterone secretion.